All about prostate cancer
Our understanding of prostate cancer has come a long way since 1853, when London Hospital surgeon John Adams first described it following surgery. And even further since the first biochemically confirmed case from the seventh century B.C.E. was found in mummified remains in Siberia.
In 1853, Adams described prostate cancer as “a very rare disease,” but that’s now thought to have been a wild underestimation, because today, one in eight men will be diagnosed with prostate cancer in their lifetime. In fact, prostate cancer is the most common cancer diagnosed in men.
But better outcomes are also more common. In the 1970s, 65% of those diagnosed were still alive five years later. Today, 91% are still alive five years later, and that number is improving annually.
What is prostate cancer?
There are four stages of prostate cancer:
- Stage 1: The cancer very small and only in the prostate. It is growing slowly.
- Stage 2: The cancer is still only in the prostate but is at risk of spreading.
- Stage 3: The cancer has spread, but not to lymph nodes or other organs.
- Stage 4: The cancer has spread to nearby or distant organs (lungs, liver, etc.) and lymph nodes, potentially to bones as well.
Sometimes prostate cancer is asymptomatic, but some symptoms might include trouble urinating; changes in urination frequency; pain or burning while urinating; blood in urine or semen; pain in the back, hips, or pelvis; or painful ejaculation. Other conditions may cause these symptoms, but it’s always best to talk to a healthcare professional when experiencing new, unusual, or uncomfortable symptoms.
What causes prostate cancer?
While the exact cause of prostate cancer is often unknown, there are certain risk factors that can increase a person’s risk of developing prostate cancer. Some of these include:
- Age — most common after age 50
- Family history — close relative(s) with prostate cancer
- Race — Black ethnicity carries greater risk
- Weight — being obese or overweight
- Genetics — certain inherited genes such as BRCA1 or BRCA2
- Height — taller men may have a slightly higher risk
How is prostate cancer diagnosed?
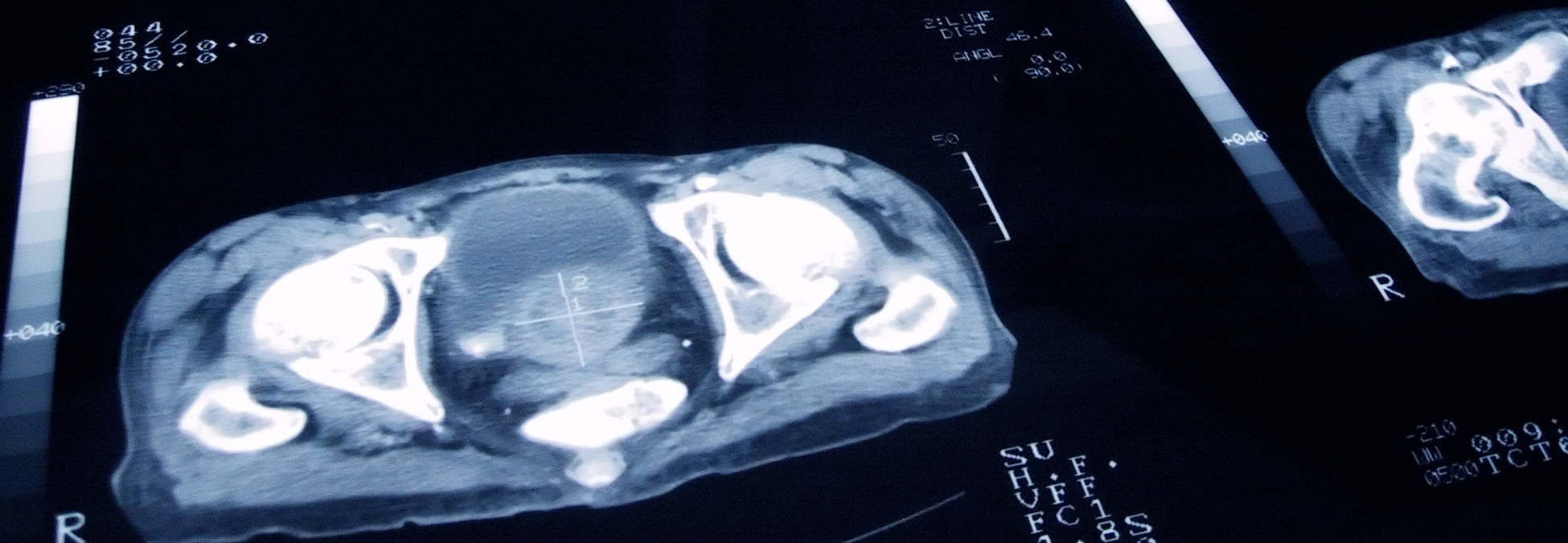
Prostate cancer is usually diagnosed after a referral to a urologist for testing to rule out other conditions. First, there will be a physical exam that may include a digital rectal exam to check the size and shape of the prostate. Certain blood tests might be done to test for markers of prostate cancer to test how certain organs are functioning to see if there are abnormalities worth investigating. Transrectal ultrasound might be used to make images of the prostate as needed, or to guide a needle used to take tissue if a biopsy is needed. An MRI or CT scan may also be used to create 3D images to check for prostate cancer that other tests might miss or to see if the cancer has metastasized or spread.
The chances of survival are very high for men diagnosed with prostate cancer at Stages 1 through 3, but they drop significantly if the cancer is Stage 4.
Regular screenings and early diagnosis are critical.
How is prostate cancer treated?
No two people are exactly alike, and no two prostate cancer cases are exactly alike. Different patients may receive different treatments depending on the stage of the disease, personal physiology and treatment preferences, age, and life expectancy, among other factors.
Treatments can include:
- Active surveillance or watchful waiting by your healthcare provider before deciding on further treatment.
- Surgery to remove the cancer.
- Radiation therapy to destroy cancer cells.
- Hormone therapy to block or lower testosterone to counteract how prostate cancer cells use hormones to grow.
- Chemotherapy to destroy cancer cells.
- Targeted therapies aimed at specific molecules on cancer cells.
- Radioligand therapy to deliver radioactive targeted therapies that destroy cancer cells.




