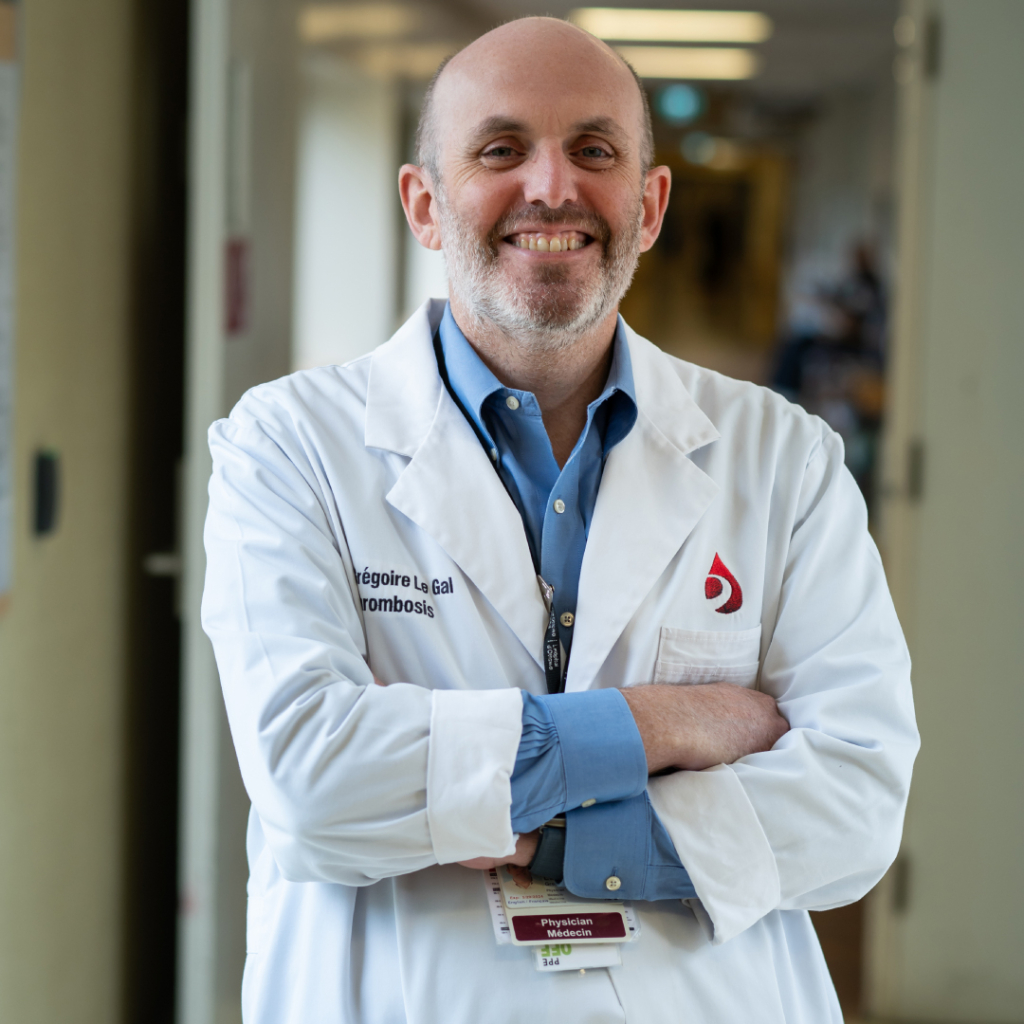
What do crepe dough and the blood of hospitalized patients have in common? Standard practice for both is to make them thinner to prevent lumps — or blood clots. But Dr. Grégoire Le Gal — physician and senior scientist at The Ottawa Hospital, and renowned crepe maker in his own home — is investigating whether giving all these patients blood thinners is as effective as we once thought. Note: he is not challenging the existing paradigm around crepes.
A general internist by training who works in hematology, Dr. Le Gal’s clinical work takes him just about everywhere in the hospital — he treats patients where they are. As he says, “there’s no place we don’t go.”
Read on to learn how Dr. Le Gal wound up at The Ottawa Hospital and what practice-changing research won him the 2024 Chrétien Researcher of the Year Award.
Q: Can you tell us a bit about your early years?
A: I’m from France, where I grew up in Brittany. My parents spoke Breton growing up, and it’s the language they dream in. It’s a different culture there: different folklore, different dances, different food. We invented pancakes and crepes! Being from Brittany resonates a bit with my experience in Canada, with the bilingualism and coexistence of cultures.
I was rather good at school, and I played sports like basketball.


Q: What did you want to be when you grew up?
A: I think I wanted to be a teacher; my parents were teachers. I also played oboe, though, almost at a professional level. When I finished Grade 12, I was studying medicine and music, and my oboe teacher said, “You can’t train to be a doctor and train to be a professional oboe player, so you’ll have to choose!”
Q: What made you originally interested in pursuing medicine — which you eventually chose over oboe playing?
A: I have a bad answer for this one. When I went to my oboe lessons, I took the bus from high school to the conservatory, and it would go by the school of medicine. It was an ugly concrete building. Every time I passed, I’d say, “That’s something I would never do, medicine. I don’t know why people do that!”

But then I graduated, and I went camping with my friends. My mom calls and says, “Grégoire! Today is the last day to register for university, and you need to do something!” I asked around my circle of friends who were with me, and a couple guys said they were going into medicine.
Once I got into the program, I thought, “I’ll do it and see.” It was a challenge not to fail. What made me realize the choice was right was that soon after I started doing night shifts as a personal support worker in a retirement home, and I loved it. I knew I was in the right place.
Q: How did you fall into doing research?
A: I am a general internist by training, so I thought I’d do general internal medicine. I didn’t want to wind up too specialized, which I wound up being anyway! But I had a defining moment when I did my first rotation in internal medicine. My mentor was doing research about thrombosis, or blood clots. It was kind of a “wow” moment, where I said, “OK, that’s what I want to be, that’s who I want to be, that is so cool.”
“It’s very powerful to enable the patient to be a part of the solution.”
— Dr. Grégoire Le Gal
It’s cool to be able to tell a patient, “I don’t know exactly what the best option is, but I have this study that’s addressing it, and together, we can get the answer.” It’s very powerful to enable the patient to be a part of the solution.
Q: Can you describe the research for which you’re receiving the Chrétien Researcher of the Year Award?
A: We know that being stuck in a hospital bed increases your risk of blood clots. We’d like to prevent that, but it’s not always clear who’s at higher risk and how to prevent it.
More than 20 years ago, they did some trials that found giving admitted patients a low dose of a blood thinner called heparin every day lowered their risk of blood clots. But the issue was, they were using ultrasounds that found a lot of small blood clots, and a lot of those might not be worth preventing. But from this, they began giving a heparin injection to every patient admitted to hospital, which is huge. For most countries in the Organisation for Economic Co-operation and Development (OECD), up to 1% of the population can be in a hospital bed at any given time, and then each of them is getting a daily shot of heparin.
But, the pendulum of medicine swings, and we thought maybe patients who were not very sick and could move and walk might be at lower risk of blood clots. We did a clinical trial to look only for symptomatic events, blood clots big enough to cause issues. We couldn’t find a significant difference in these clots between admitted patients who got daily blood thinners and those who did not. It’s a tricky study, though. Some studies are very easy; the results are very clear. But for this study, it looked like some patients might benefit. We haven’t fully answered the question yet.
Q: How will this research help patients at The Ottawa Hospital — and beyond?
A: If it was confirmed that a lot of admitted patients do not benefit from daily blood thinners, the cost savings for the hospital could be huge. These are expensive medications.
For patients, a lot of patients don’t like being poked every day. It is a common theme, where older adults feel that it’s aggressive to get an injection every day, so this could improve patient comfort.
And from a staffing perspective, it’s one less visit from a nurse, reducing their workload.
Q: How did it feel to receive this award?
A: Great, actually. It’s a prestigious one, and good friends and mentors have received it before me. I have a bit of imposter syndrome as well, because it was not a study that I directly led, I was mentoring it and supervising it. Pride, though, for sure, and within the institution, it’s something that’s highly regarded.
Q: Why did you choose to work at The Ottawa Hospital?
A: On my path to becoming a thrombosis researcher, one of the steps was to do a post-doctoral fellowship in an English-speaking country. I was looking at Australia and Canada. And Canada is one of the top, if not the top, countries in the world, for thrombosis research. My specific interest was diagnosis. I knew about Dr. Philip Wells, he’s world famous for his Wells Score for diagnosing deep vein thrombosis. So, I came to him and said, “Hey, would you take me for a year?” I had just a great time, from a family and from a work perspective.
“Not many hospitals have such a sophisticated system for thrombosis, which means we see pretty much each and every blood clot in the entire Ottawa region.”
— Dr. Grégoire Le Gal
From a thrombosis research perspective, it’s quite unique what we have in Ottawa. With Dr. Marc Rodger and Dr. Wells, we have pioneers here. Not many hospitals have such a sophisticated system for thrombosis, which means we see pretty much each and every blood clot in the entire Ottawa region.
Q: Can you speak to the role of international collaboration in your field?
A: In Canada, they set up a network of all the thrombosis research teams and centres, and when I was in France, we did the same. When I came to Canada, I had a mission to unite the two. The Canadians work with the French because we have a lot in common, and now we have an international network with the Netherlands, Italy, Spain, the US, China, Uruguay, and more. The idea is that if one group, say the Dutch, has a study they want to do, but they don’t have enough patients, they come to the network and ask if someone else can do the study. I spent a lot of time building these relationships and trying to streamline international collaboration, which can be very difficult, because we’re very siloed by country. I’m the director of the Canadian one, which is called CanVECTOR, and was chair of the international one previously; it’s called Invent VTE.
Q: What is The Ottawa Hospital doing in thrombosis research that is exciting or groundbreaking?
A: What’s exciting is that, now, we have a very large group of thrombosis researcherS. There are 11 or so of us. We study in fields where not many go. There are experts in cancer-associated thrombosis. There are teams looking at preventing blood clots with pills in patients with cancer. We’re doing another trial now for patients who get PICC lines or port-a-caths, because there’s a risk of clotting when they put it in. In yet another trial, we’re comparing two blood thinners from two different pharmaceutical companies. Each says theirs is better, but no one’s ever compared them before. Others on the team are doing exciting work on the risk of bleeding, on perioperative management, on patient engagement in research, on screening for cancer in patients with thrombosis, on ethnoracial diversity (or the lack thereof) in thrombosis research etc.
You will see many researchers of the year coming from the thrombosis group in the years to come.
Q: Where would we find you when you’re not at work?
A: You could find me on my bike. That’s another reason to like Ottawa, all the bike paths everywhere. I travel a lot. My wife is from Ecuador, South America, and I have cool kids. It’s funny to see them grow — they’re 20 and 18. When they’re younger, you’re like, “Maybe when they’re older, they’ll change.” Then they grow, but they remain your little kids. I find it amusing how much I enjoy being a dad.



I also love making crepes. I had to have an electrician do a custom outlet in my house in Ottawa so I could continue to use my crepe machine from France. It’s a nice thing to invite friends and people for. Everybody stands up in the kitchen around the machine. You need to make them very thin and very flat. There’s a technique, and everyone wants to try it. It’s a very friendly type of meal.



