A CANCER JOURNEY
A journey through two cancers and the BRCA gene mutation
Update February 2026:
Jennifer recently surpassed the five-year milestone since first being diagnosed with ovarian cancer on July 29, 2020. Then, in January she also celebrated the five-year milestone since completing chemotherapy. During her treatment, she underwent a bilateral mastectomy due to her high risk of breast cancer and has now completed a series of breast reconstruction surgeries. Jennifer is doing well and it glad to be able to focus on the future.
Published: February 2025
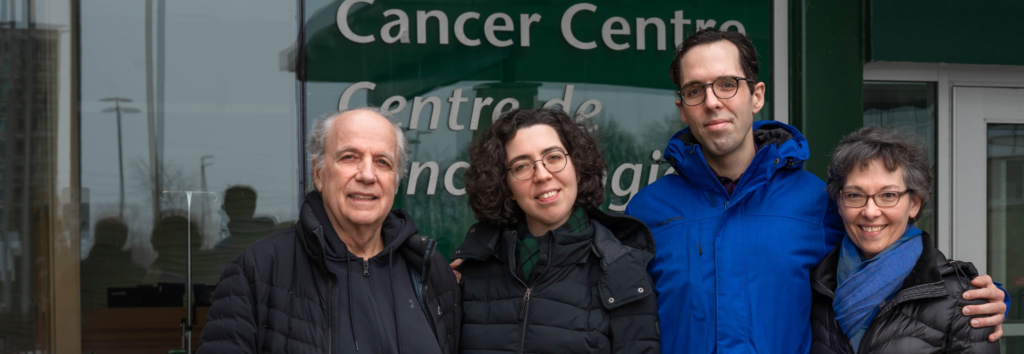
When Jennifer Hollington was diagnosed with ovarian cancer, she didn’t see it coming. This shocking news started her down a path she never imagined, including two more significant medical developments: the discovery she had the BRCA2 gene mutation, and a skin cancer diagnosis.
While well-versed in the healthcare sphere because of her job with Health Canada and the Public Health Agency of Canada, Jen wasn’t prepared for the health crisis she faced in 2020 at the height of the pandemic. However, she was introduced to a large multidisciplinary team of healthcare professionals at The Ottawa Hospital, who helped guide her through this cancer journey.
It was late July 2020 when Jen woke up in the middle of the night with intense pain in her side. After a call to Telehealth Ontario, she went to a local Emergency Department, where blood work and an ultrasound revealed the shocking news — Jen’s tests pointed to a likely diagnosis of ovarian cancer.
“It was a scary and unexpected diagnosis. I came to terms with it only after repeating it many times to family, friends, and co-workers,” she explains.
A stage 3 ovarian cancer diagnosis
By early August, Jen took a leave from her job as the Assistant Deputy Minister of Communications for Health Canada and the Public Health Agency of Canada. Not long after that, she met Dr. Wylam Faught, head of the division of gynecologic oncology based at the Shirley E. Greenberg Women’s Health Centre at the Riverside Campus.
“He sees you as a person, not simply as a patient who is on a long list of patients.”
— Jen Hollington
Dr. Faught took time to walk Jen through what her journey might look like with what he suspected was stage 3 ovarian cancer. “We’re pretty realistic when meeting with a patient who faces this diagnosis. We try to start into the treatment journey with the patient’s eyes wide open — every patient is different.”

For Jen, this approach was exactly what she needed. “Dr. Faught was very empathic, but also realistic about the challenges of ovarian cancer, which I appreciated. He sees you as a person, not simply as a patient who is on a long list of patients. It was comforting to know that we were moving forward, but it was also scary.”
The impact of research on patients facing ovarian cancer
In 2024, an estimated 3,000 Canadian women were diagnosed with ovarian cancer. The disease impacts women of all ages, but it’s more common in women who have gone through menopause. Sadly, the current five-year survival rate is only 45%, and that’s why research at all levels plays a critical role in advancing new treatment options.
Researchers like Dr. Barbara Vanderhyden and her team at the Vanderhyden laboratory at The Ottawa Hospital are dedicated to studying this disease.
Testing shows the BRCA2 gene mutation
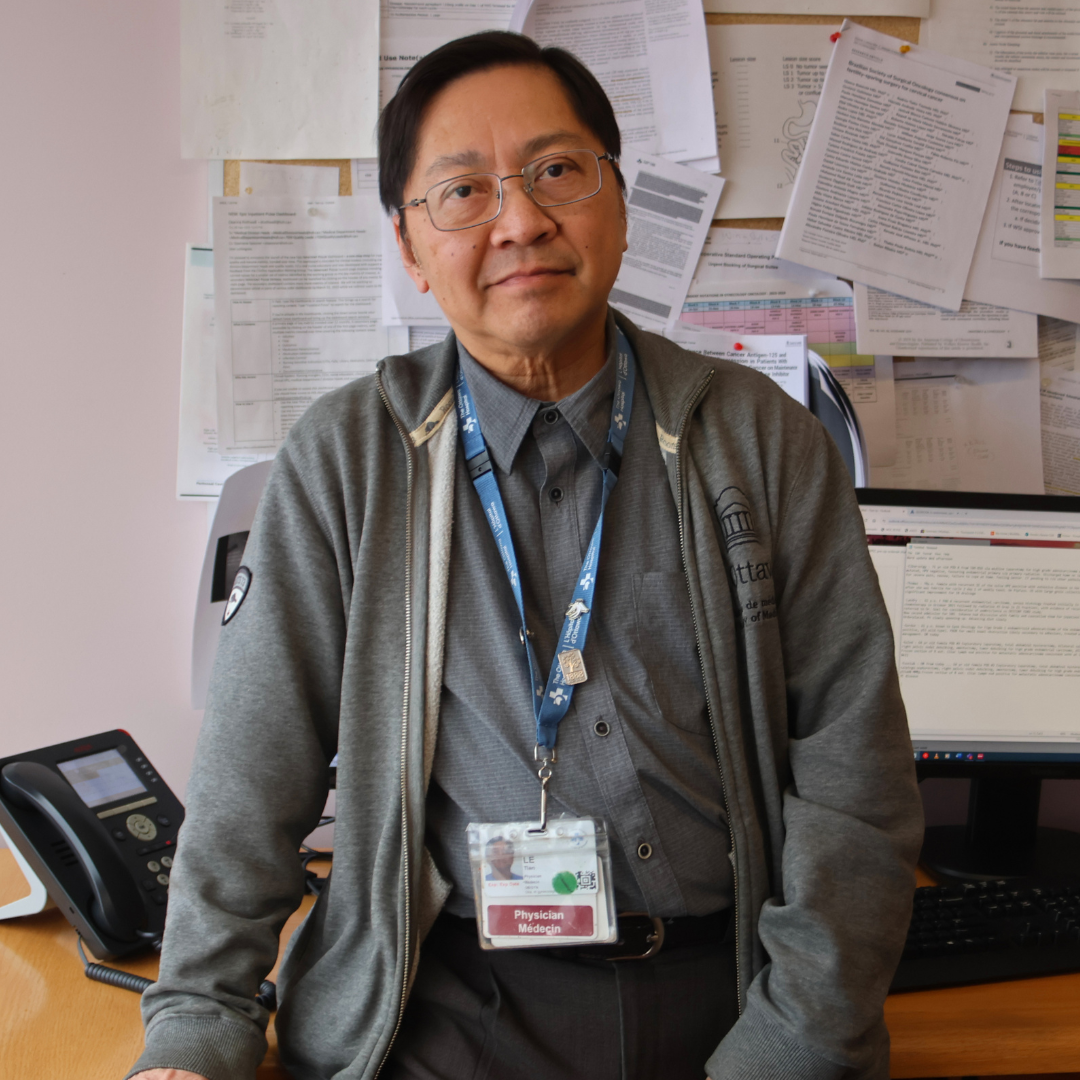
In late August, Jen underwent surgery to remove her uterus, cervix, ovaries, and Fallopian tubes, followed by six rounds of chemotherapy. Her gynecologic oncologist, Dr. Tien Le, was able to remove most of the visible cancer. The final pathology report confirmed Jen had stage 3 high-grade serous carcinoma arising from her ovary. Luckily, this meant there were very good initial treatment options to manage her cancer.
“Dr. Le told me they are increasingly looking at ovarian cancer as a chronic disease, to keep people living longer and longer. I found this especially encouraging,” says Jen.
That pathology report also indicated her ovarian tumour cells carried the BRCA2 gene mutation. Genetic testing was suggested to see if she was a carrier of the gene change. This would have further impact on immediate family members and direct further treatment for the patient.
All humans have the BRCA genes (BRCA1 and BRCA2). You inherit one from each of your parents, and if one parent has a mutation, there is a 50% chance you will inherit it. These genetic mutations are known to predispose carriers to develop hereditary breast and ovarian cancers, among other cancers.
“Patients with this mutation tend to have a much better prognosis than someone who is not a carrier of the gene change, because there are more treatment options, and the patient is more responsive to chemotherapy. It was positive news overall.”
— Dr. Wylam Faught
By the spring of 2021, genetic test results showed Jen had a mutation in her BRCA2 gene, which subsequent testing revealed she had inherited from her father. This presented another medical hurdle, namely a significant risk of developing breast and other cancers.
While the news was initially alarming to Jen, Dr. Faught explained it offered hope. “Patients with this mutation tend to have a much better prognosis than someone who is not a carrier of the gene change, because there are more treatment options, and the patient is more responsive to chemotherapy. It was positive news overall.”
Once her chemotherapy was complete, Jen was eligible for an effective new class of oral medication known as PARP inhibitors called Olaparib. “It’s only been in the last handful of years that this group of patients with the BRCA gene mutation have benefitted from this new drug, which in some cases has the potential for putting them into remission. So, within her diagnosis of ovarian cancer, there was this silver lining,” explains Dr. Faught.

Optimizing her chances for the future
With the results of the genetic testing placing Jen at a higher risk of breast cancer, Dr. Le referred her to Dr. Erin Cordeiro, a breast surgical oncologist at The Ottawa Hospital.
“Dr. Cordeiro was clear, respectful, and kind as she answered all my questions and provided the detailed information I needed to make my final decision on one of two options,” says Jen.
Those options included continuing with annual mammograms and breast MRIs through Ontario’s high-risk screening program or having a preventive bilateral mastectomy. Armed with plenty of statistics, like how preventive surgery would reduce her risk of developing breast cancer by 95%, Jen considered the options.
“I pretty much knew right then and there, surgery was the best option for me. I was so reassured by the call with Dr. Cordeiro. I came away knowing so much more about my options as well as their advantages and disadvantages.”
Her next step was to meet with a plastic surgeon, because as Dr. Cordeiro explained it, she would remove the breast tissue and the plastic surgeon would reconstruct the breasts during the same surgery.

Then another cancer diagnosis
Shortly before the appointments relating to her mastectomy, Jen inquired with her family doctor about an itchy patch of skin near her anus that had persisted for a few years but seemed harmless enough. In September 2021, she met with a dermatologist, who did a biopsy. “He mentioned the possibility of cancer. I thought ‘Good grief, as if I need more cancer in my life.’”
Within days, the news was confirmed, Jen had a second cancer — anal margin squamous cell carcinoma — perianal skin cancer. This news introduced her to a whole new cancer team at our hospital who rallied around her.
Colorectal surgeon Dr. Robin Boushey removed an almost one-centimeter tumour. When the post-surgery pathology report indicated that pre-cancerous cells remained in the margins, Dr. Boushey referred Jen to radiation oncologist Dr. Jenny Jin.
“The pathology showed there were precancerous tumours along the cut edge of the tumour. We knew that she would have quite a high risk of local recurrence if there was no further treatment,” explains Dr. Jin.
“There’s been no evidence of any recurrence, and soon she’ll be three years out. The highest rates of recurrence are in the first two years, and so her chances are getting better.”
— Dr. Jenny Jin
Another surgery was possible, but that brought some risks and could impact Jen’s quality of life. “If she were to have more resected, it would mean that she’d likely end up with a permanent ostomy pouch for bowel movements, so we went with an organ preservation approach,” explains Dr. Jin.
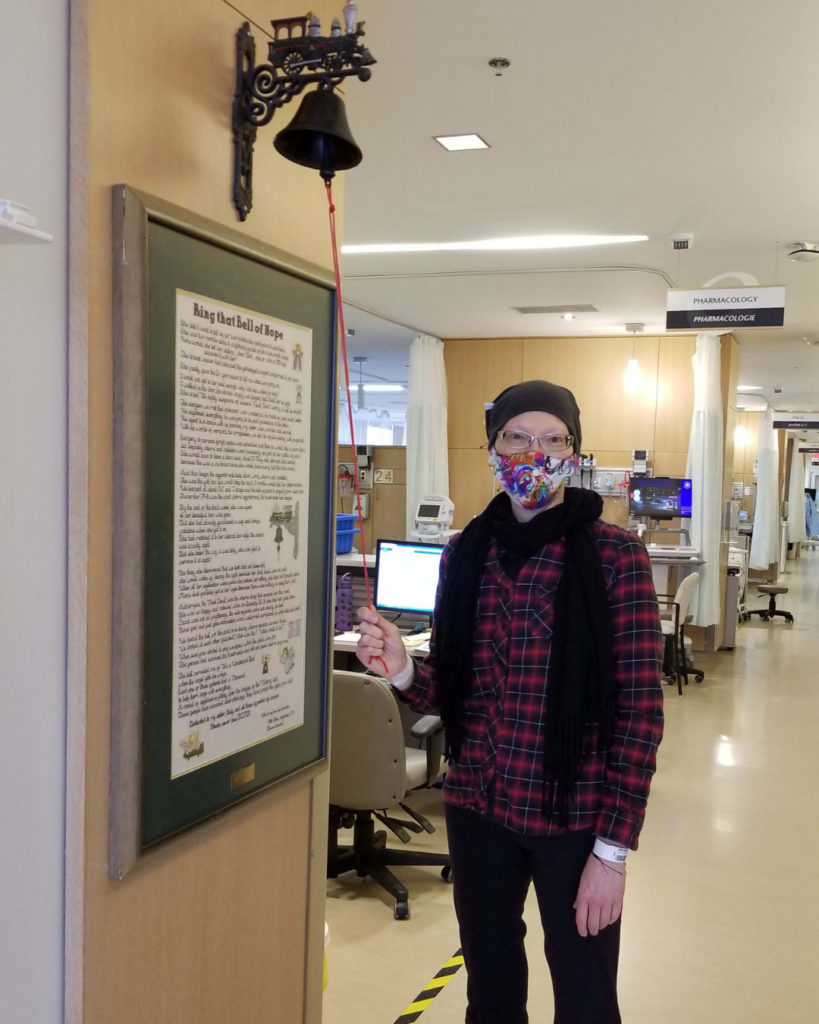
By February 2022, Jen finished 25 treatments of radiation. “She’s done very well ever since. There’s been no evidence of any recurrence, and soon she’ll be three years out. The highest rates of recurrence are in the first two years, and so her chances are getting better,” says Dr. Jin.
For Jen, it was another big hurdle she’d overcome.
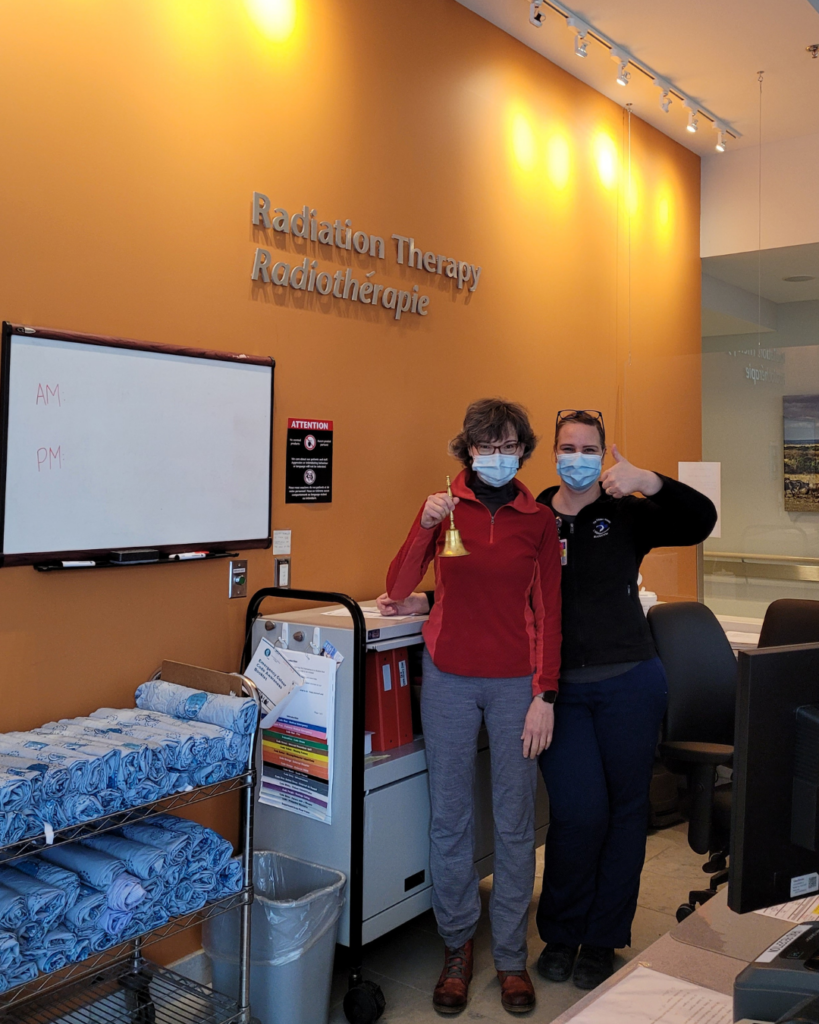
The overarching support along the way
One thing that stands out to Jen along this journey has been the many multi-disciplinary teams who cared for her, including many nurses and allied health professionals. One in particular had a huge impact. Jacinthe Lepage has been a nurse at The Ottawa Hospital for over 30 years, and she’s spent most of her career working in gynecology oncology.
More recently, her role has evolved to include a first-of-its-kind nurse-led PARP inhibitor clinic at our hospital’s Cancer Centre.
“The clinic first opened in March 2023 and there’s no other clinic like it – anywhere in Canada,” explains Jacinthe. “There’s a lot of monitoring and calls when somebody is on this drug, so I’m the nurse that’s there for those patients.”
It’s this experience, compassion, and candor that Jacinthe brings to patients that resonated with Jen. “Jacinthe is fabulous, and she’s been with me through this whole experience. A voice of comfort and reason when I have questions. She’s always there.”

“I don’t see the cancer when I talk to them, because I know that they don’t want to be identified as that. To me, it’s very important to treat the person behind all this.”
— Jacinthe Lepage
For Jacinthe, it’s a special role that she takes very seriously, and it’s different for each person. “We treat the cancer, but I see the person behind all this. I don’t see the cancer when I talk to them, because I know that they don’t want to be identified as that. To me, it’s very important to treat the person behind all this.”
As she explains, they need to be able to open up and ask any questions. “I know some are afraid to ask questions about death and dying, about prognosis and all that, but I always tell myself, if they have the guts to ask, I can’t hide anything. When they ask, it’s because they are ready for the answer.”
Hope for patients in the future facing an ovarian cancer diagnosis
Four-and-a-half-years after this cancer journey started, Jen remains cancer-free. There have been some bumps in the road, including with her breast reconstruction surgery — a process that continues. She’s even offered hope and guidance to others through the blog she started, Jenesis, which has also been therapeutic for her.
“At this point, with no evidence of disease, the risk of recurrence is quite low. Dr. Faught estimated my risk of recurrence to be less than 10%. I almost cried when he said that.”
— Jen Hollington
In November 2024, she reached a significant milestone when doctors recommended she come off the PARP inhibitor drug, which suppresses the growth of cancerous ovarian tumours. “There’s no evidence that staying on the drug would have a long-term benefit beyond two years,” explains Dr. Faught.
It was a challenging decision for Jen, as there was comfort in knowing she was taking this drug and doing well. “At this point, with no evidence of disease, the risk of recurrence is quite low. Dr. Faught estimated my risk of recurrence to be less than 10%. I almost cried when he said that, remembering that he had told me in August 2020 that the risk of recurrence in ovarian cancer is about 80%,” shares Jen.
According to Dr. Le, there is new hope on the horizon for patients with ovarian cancers. “We are embarking on a new program at The Ottawa Hospital to advance the care and improve survivals for ovarian cancer patients in the form of HIPEC treatment. This involves administering heated chemotherapy solution right into the abdominal cavity at the time of surgery for their cancers. This strategy has been shown to significantly improve the survival for patients with ovarian cancer in selected cases.”
While more and more centres are adopting this therapy, The Ottawa Hospital would be only the second hospital in Ontario to provide it to patients. It’s new advancements like this one that give patients like Jen hope for more effective treatment options and better survival.
As Jen moves forward, she embraces parts of life that she may not have noticed before. “Special moments that once may have seemed mundane have become clearer and brighter as I live each day, grateful that I am still here.”