
All about kidney disease
If our bodies were cities, the kidneys might be our water treatment plants. Filtering about 125 mL of blood per minute, the kidneys clean our blood and return it back to our arteries, turning the waste products and extra fluid into urine.
But the kidneys do much more than just filter waste; they also help make red blood cells and regulate blood pressure. With all they do, it might be surprising to know most people only need one functioning kidney to live. But what happens if you don’t have enough functioning kidney tissue?
What is kidney disease?
Chronic kidney disease — also called CKD or nephropathy — occurs when the kidneys are damaged or not functioning properly and cannot filter blood as effectively as they should. This causes waste to build up in the blood. Approximately one in 10 Canadians has kidney disease, or about four million Canadians.
What causes kidney disease?
Diabetes is the most common cause of kidney disease. In fact, 38% of all kidney disease is caused by diabetes and 50% of people with diabetes experience kidney damage at some point. Other common causes of CKD include high blood pressure, autoimmune diseases, inherited health conditions, malformations in the urinary tract or kidneys before birth, damage from kidney stones, and medication toxicity.
How is kidney disease diagnosed and treated?
CKD is diagnosed by a blood or urine test that measures how well your kidneys are functioning. If left untreated, CKD can lead to kidney failure.
There are five stages of CKD, which are based on how well the kidneys are filtering blood. In stages 1 and 2, the kidneys are still cleaning the blood at over 60% capacity; by stage 3 there is moderate to severe kidney damage and kidney function will drop below 60%; and stage 5 is classified as kidney failure, with the kidneys cleaning the blood at less than 15% capacity.
In the early and mid-stages, doctors focus on interventions such as lifestyle changes and possibly medication. But by stage 5, kidney failure, there are two treatments options: dialysis or a kidney transplant.
What is dialysis?
Dialysis is a way to clean your blood when the kidneys no longer can. Usually, people who start dialysis due to kidney failure have to continue it for life, unless they receive a transplant. Dialysis can be delivered in a hospital, but it can also be offered in a community setting like a clinic, or even at home. Read more about Home Dialysis Program below.
Drainage Fluid
Drain bag with removed waste
Roller Pump
Dialyser
Used dialysis fluid with removed waste
Dialysis fluid
Clean fluid
Blood
Drainage fluid
Drain bag with removed waste
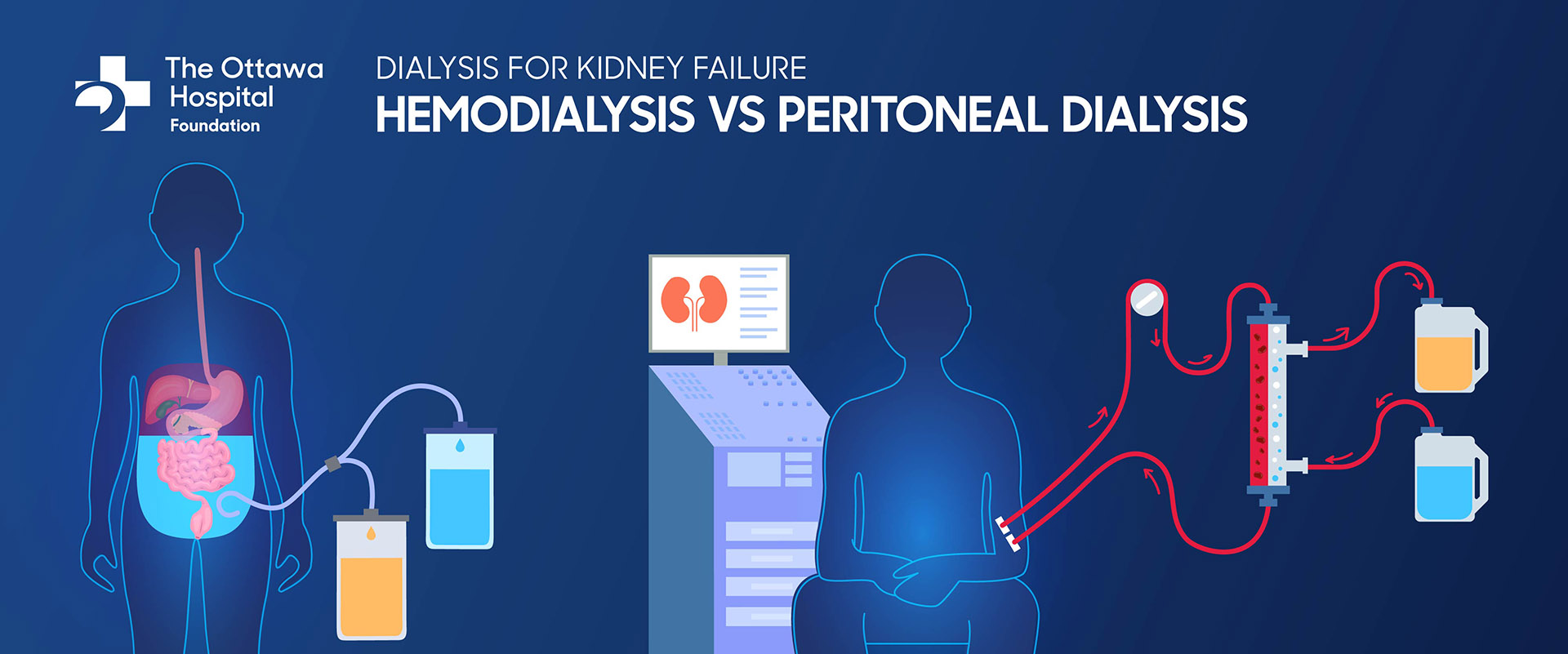
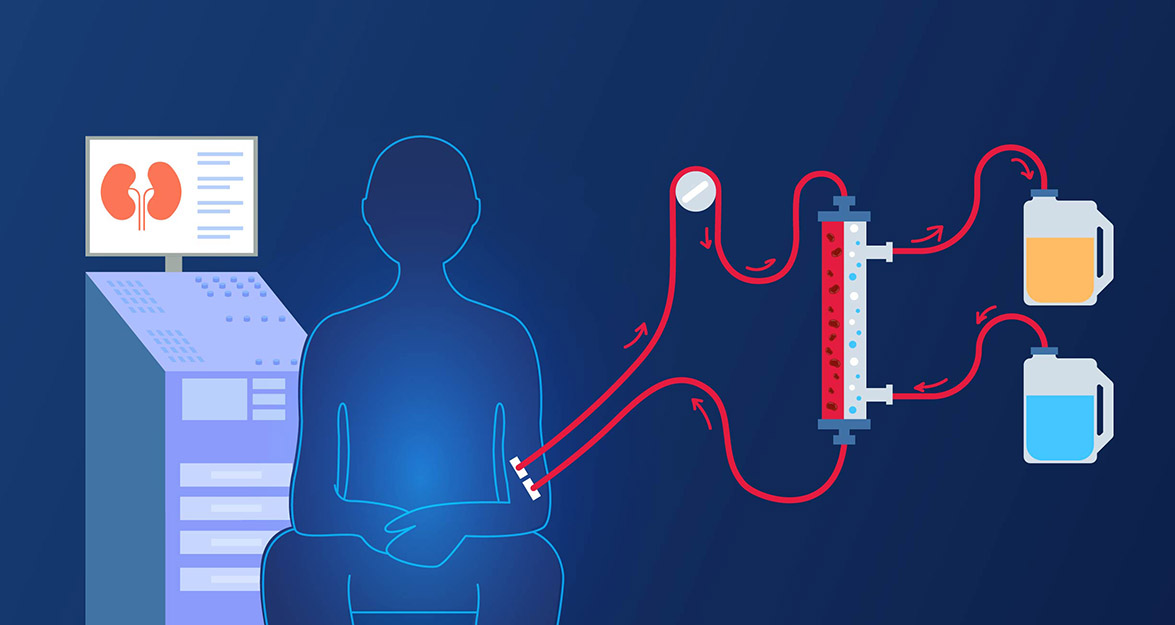
Peritoneal Dialysis
- Drainage fluid flushes the abdominal cavity, removing waste from blood
- Must be done daily
- Portable option, patient can go about daily life during treatment
Roller pump
Dialyser
Used dialysis fluid with removed waste
Dialysis fluid
Clean fluid
Blood
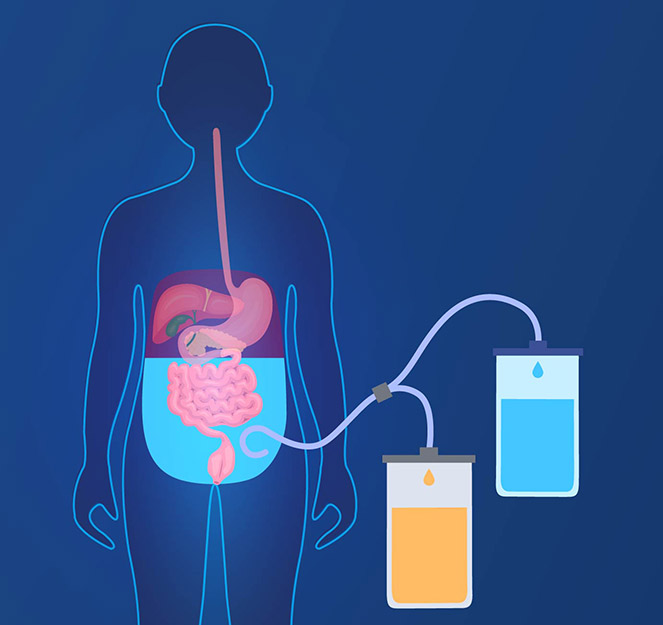
Hemodialysis
- Blood is cleaned through a machine, up to three times a week
- Can be done at home, at an outpatient clinic, or in hospital, but patient must remain stationary for treatment
What are the symptoms of kidney disease?
In stages 1 and 2, CKD has few symptoms. However, from stage 3 onwards, symptoms might start appearing, such as:
- tiredness
- poor appetite
- itching
- trouble concentrating
- trouble sleeping
- nausea
- muscle cramps at night
- swollen feet, ankles, or puffiness around the eyes
- trouble breathing
- needing to urinate more or less often
What is The Ottawa Hospital doing in kidney disease?
Our team is always working on practice-changing research and offering the most current care for kidney disease.
We offer the Home Dialysis Program, which is one of the largest home dialysis programs in North America, with more than 220 patients receiving home dialysis through the program currently. It uses a holistic approach, with a team of nephrologists, nurses, dieticians, and social workers. The most common form of dialysis in this program is peritoneal dialysis, and the program allows patients to tailor their treatment to their schedules and needs better, from the comfort of their own home.
We also offer in-centre dialysis at our Civic and General Campuses, with the Riverside Campus offering another out-patient unit. There are also six satellite units located at Bruyère Continuing Care, Hawkesbury, Queensway-Carleton Hospital, Winchester, and the eastern Ontario/Cornwall and Ottawa-Cornwall dialysis clinics. We currently have over 650 patients in our chronic hemodialysis program.
Kidney disease research at The Ottawa Hospital
Established in 2000, our Kidney Research Centre (KRC) is Canada’s first research facility devoted exclusively to investigating diseases that attack the kidneys. KRC scientists and clinician researchers are taking a lead role nationally in developing new strategies to improve detection and treatment of kidney disease.
Our dedicated Jindal Research Chair for the Prevention of Kidney Disease position is helping kidney disease stay front and centre at The Ottawa Hospital. In his role as the inaugural chair and Senior Scientist and Nephrologist at The Ottawa Hospital, Dr. Manish Sood authored over 200 research papers, gave over 50 invited lectures, and conducted research on using “big data” to prevent and treat kidney disease.
In 2023, a new chair was announced: Dr. Edward Clark. Dr. Clark knows how devastating critical illness can be for the kidneys, and he specializes in caring for the 10% of patients in the ICU whose kidneys stop working. As new chair, Dr. Clark will accelerate his research, which aims to help more critically ill patients survive acute kidney injury and recover enough kidney function to avoid ongoing dialysis.
When you support The Ottawa Hospital, you support the best care for patients with kidney disease and the critical work being done by Drs. Sood and Clark and their teams — helping people live longer and healthier lives with kidney disease, treating kidney disease, or even preventing it in the first place.





