When a routine mammogram identified a small tumour, Rita Nattkemper was given an innovative option to mark its location for the surgery. A radioactive seed, the size of a pinhead, was injected directly into the tumour in her breast.
“All I have to say is it’s a painless procedure to get this radioactive seed in and it helps the doctor with accuracy,” said Rita. “And as he removes the mass, he’ll be removing the seed at the same time.”
For the last 20 years, when a woman had a breast cancer tumour that was too small to feel or be seen in surgery (called a non-palpable tumour), she had to have a wire (known as a harpoon) implanted at the tumour site to locate it for the surgeon. The wire, which stuck out of the woman’s breast, had to be inserted the morning of her surgery. Then, women had to wait uncomfortably for surgery with the wire sticking out of their breast. To add to the discomfort, many women had to fast overnight to prepare for surgery, causing many to faint in the radiology suite at the sight of the wire protruding from their breast.
The procedure also posed other problems.
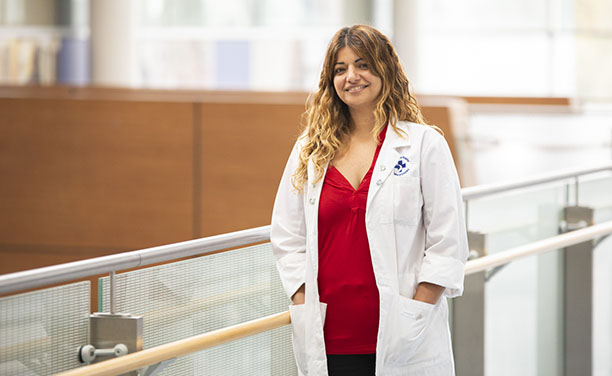
“Sometimes the wire moved. And sometimes, because of the location of the tumour, the wire might overshoot or undershoot the tumour, so ultimately there was an enormous amount of guess work involved in taking out a breast cancer tumour properly,” said Dr. Carolyn Nessim, surgical oncologist, and clinician-investigator in the Cancer Therapeutics Program at The Ottawa Hospital.
Dr. Nessim, and other breast oncology surgeons, wanted to find a better option.

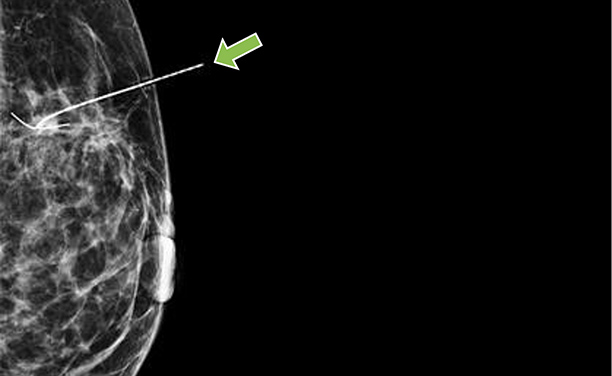
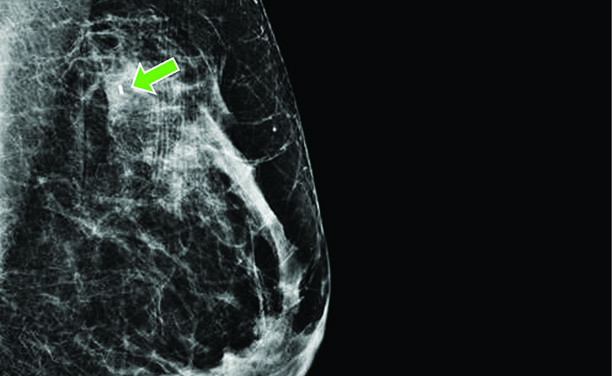

That was where radioactive seeds came in. Radioactive seeds have been used for many years to treat prostate cancer. Multiple seeds are implanted in the prostate, where they emit radiation and kill the cancer. Then a procedure was developed for breast cancer patients using a radioactive seed to mark the exact location of small breast-cancer tumours. Using a mammogram for guidance, a radiologist places one seed, so tiny it can be safely injected with a needle, inside the tumour. It emits a very small amount of radiation that is picked up in the operating room with a small, handheld Geiger counter. After the piece of breast tissue with the radioactive seed is removed, the seed is separated from the tissue and appropriately disposed of, with every seed being accounted for.
Realizing the benefits of this procedure, The Ottawa Hospital began a radioactive seed program in 2015. One of the main benefits is that the seed can be placed up to a week before surgery, which makes the day of the operation easier for patients. A woman doesn’t have to wait for surgery with a wire sticking out her breast. From a logistical point of view, it’s easier to organize the procedure days in advance, and means more efficiency in the operating room. Dr. Nessim led a research study comparing seeds to wires, which showed the benefit of seeds.
“The results of the radioactive seed program have been uniformly excellent,” said Dr. Erin Cordeiro, breast surgical oncologist and senior clinician-investigator at The Ottawa Hospital. “We did a study that found that radioactive seeds were more cost effective and decreased wait times for patients on the day of surgery when compared to wires. And the patient experience has also been wonderful. Patients are very supportive of this.”
Rita agrees. She said the surgeon and radiologist both explained the procedure and put her at ease about it.
“I felt a minor pinch, and that was all I felt,” Rita said immediately after the procedure. “And the radiologist had the screen turned, so I could see where she put in the needle and left the seed. It was very easy, very quick, and very painless.”
Dr. Cordeiro said women are often concerned about the seed’s radioactivity, but the staff reassures patients the procedure is completely safe. The amount of radiation that is emitted in the week the patient has the implanted seed is less than having two mammograms.
“A woman can continue to hug her children and do everything in life she would normally do,” said Dr. Cordeiro. “No concerns from that point of view. It’s an extremely safe procedure. The vast majority of women have no concerns.”
Over the past year, 355 radioactive seed procedures have been performed at The Ottawa Hospital. Only two patients have refused the seeds and opted for the traditional wire instead.
Because of the program’s radioactive element, there were stringent guidelines around starting the program.
A multidisciplinary team of nuclear medicine, radiation safety experts, radiologists, pathologists, surgeons, technicians, and nurses were involved.
Key members of the team, led by Dr. Nessim, went to the Mayo Clinic in Rochester, N.Y., to learn how to implement the program. They then ran 15 training sessions for staff at The Ottawa Hospital. The radioactive seed program now “runs like a well-oiled machine,” said Dr. Nessim.
The Ottawa Hospital was the third centre in Canada to have a radioactive seed program, and is a leader in the procedure. Other health centres across the country are now adopting it and looking to The Ottawa Hospital for guidance in successfully implementing their program.
The Ottawa Hospital is a leading academic health, research, and learning hospital proudly affiliated with the University of Ottawa.