Originally published: February 2021
Updated: December 2025
As of November 2025, Casey is doing incredibly well. She continues to teach kindergarten and is now a mother of two — a growing family she says wouldn’t have been possible without the lifesaving care she received at The Ottawa Hospital.
Updated: July 2022
When Casey Delaney was struck by an out-of-control personal watercraft two years ago, her life came to a sudden stop. Having sustained a severe traumatic brain injury, doctors weren’t sure if she’d be able to walk, talk or return to her passion for teaching, ever again. But thanks to specialized rehab therapy at The Ottawa Hospital’s Rehabilitation Centre, Casey was given the opportunity to get her life back on course.
The accident that changed everything
On Canada Day in 2018, Casey and her friends were sitting on an inflatable raft near the Gatineau River shoreline when the driver of a nearby personal watercraft lost control, hitting Casey and leaving her immediately unconscious.

Her boyfriend at the time, Scott, performed CPR until the paramedics arrived and Casey was rushed to a local hospital. However, her injuries were extensive and complex, so she was quickly transferred to our Trauma Centre at the Civic Campus for lifesaving treatment.
To reduce swelling in her brain, doctors carefully removed the left half of Casey’s skull – which was later replaced with titanium mesh – and put her in a medically-induced coma. Casey was diagnosed with a severe traumatic brain injury and her medically induced coma was extended for two weeks. Her doctors weren’t sure if she’d ever be able to walk, use her arms, or remember her loved ones. But when Casey woke up, there was hope.
“I had issues with walking at first, but I was getting up as soon as I could, and that’s pretty lucky,” says Casey, who was just 26 at the time. Lucky as she was, Casey wasn’t left completely unscathed. She had newfound weaknesses on the right side of her body and issues with memory and balance that required special care.
But our experts were ready to help Casey work through these challenges and give her the chance to return to life as she knew it.
A long road ahead
In August 2018, Casey was transferred to our specialized brain injury rehabilitation program, one of only a handful like it in Ontario, that treats patients from all over eastern Ontario and as far as Nunavut. It was there that Casey participated in two months of intensive therapy, followed by what was expected to be years of outpatient rehab.
Those who survive a traumatic brain injury are often faced with life-long side effects – both physical and cognitive, that can prevent them from living independently or participating in social activities, and can cause changes in personality and behaviour. Rehabilitation can help a person regain function in these areas, and our specialists work with patients for the duration of what can be a long road to recovery.

“If you break your leg, you might expect recovery to take about three months. Brain injury is probably one to two years of ongoing recovery,” explains Dr. Shawn Marshall, physiatrist and division head of physical medicine and rehabilitation, who worked closely with Casey throughout her care. “Because Casey had a severe traumatic brain injury, her prognosis for return to full-time work was less than 50 percent.”
Casey, a passionate kindergarten teacher, wasn’t going to let this prognosis hold her back from getting back to life, and the classroom, as soon as she could.
“I was like, ‘They’re wrong. I’m going back to teaching in September,’ which to be clear, I was not back in September,” says Casey. But, she was ready to give it her all.
Setting the stage for recovery
For patients like Casey, their care in the Trauma Centre sets the stage for their journey to recovery. Ongoing research happening right here at our hospital can help inform and improve this care.
At the time of her admission, Dr. Shane English, an ICU physician and researcher at The Ottawa Hospital, was recruiting participants for an international research trial that was investigating how to manage low blood levels in patients with a brain injury – and Casey was the perfect candidate.
“This study was brought here to truly provide the best care possible to our patients.”
– Dr. Shane English

Typically, blood transfusions are only given to trauma patients with very low red blood cell levels (anemia). However, those with brain injuries are more susceptible to low hemoglobin levels and researchers were examining whether transfusions should be given more liberally to prevent significant anemia and how this might lead to improved outcomes.
“Our job is to preserve everything we can to give them the best chances of a recovery later,” says Dr. English. “We’ve been really active in brain injury and trauma research and this study was brought here to truly provide the best care possible to our patients.”
Getting back on her feet
Throughout her rehabilitation, Casey was fortunate not only to have access to the latest cutting-edge treatments, but also to be cared for by an extensive and collaborative care team of experts, including nurses, physiotherapists, occupational therapists, psychologists, social workers, speech-language pathologists, and physiatrists.
“The most effective therapies are the ones that are meaningful to you, that engage you, and that are practical to you. Rehabilitation is about getting your life back.”
– Dr. Shawn Marshall
These experts, many of whom are involved in establishing the guidelines and best practices for traumatic brain injury care and management in Ontario, helped Casey through daily, three to five-hour intensive therapy sessions. Because no two brain injuries are alike, Casey’s care team developed a highly customized rehabilitation program that focused on improving areas where her injury caused difficulties so she could regain function and return home.
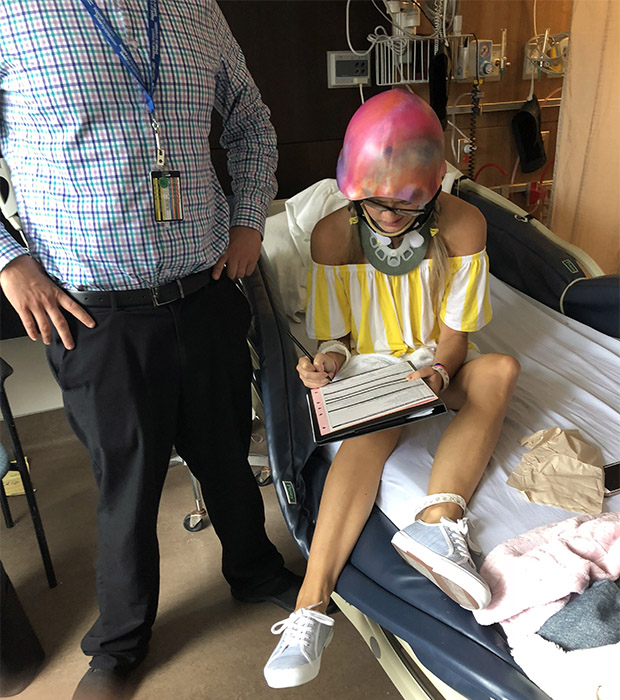

In some of her therapy sessions, Casey was taken into specialized rooms that mimicked areas of a home, like a bathroom and kitchen, to learn strategies to overcome her injury. Looking back, Casey remembers being surprised by some of the therapy sessions she participated in, which included activities like cooking and woodworking.
“Dr. Marshall was amazing and always had the next step ready to go. That’s what my brain needed.”
– Casey Delaney
“I had fine motor type classes, which seemed silly to me at the time. I teach my kindergarten students fine motor skills, but looking back, that was something I struggled with,” says Casey with a laugh. “I remember being so proud that I was able to bring home a meal I’d cooked and present it to Scott, which I hadn’t done in ages.”
While activities like cooking may seem simple, our experts say they are complex tasks for the brain and played an integral role in Casey’s rehabilitation. “When you do therapy, the most effective therapies are the ones that are meaningful to you, that engage you, and that are practical to you,” explains Dr. Marshall. “Rehabilitation is about getting your life back.”
An exceptional recovery
After only two months of therapy, Casey had made great progress in her rehabilitation and was ready to take the next step – going home. “By September I was out of the hospital and at home. That was huge,” says Casey. There was even more reason to celebrate when Scott, who had been by Casey’s side throughout her recovery, proposed.
Casey continued with daily therapy at our hospital, which became less frequent as she improved. Amazingly, by the following September, Casey was back to work full-time, doing the things she loves and no longer needed therapy.
In addition to support from her family, Casey credits her care team for giving her the tools and care she needed to bounce back, beat her prognosis, and have the opportunity for a healthy future. “Dr. Marshall was amazing and always had the next step ready to go,” says Casey. “That’s what my brain needed.”
For our experts, her recovery was nothing short of exceptional.

“The take-home of her case is how you can be drifting on a river and one second later your life is turned over and affected for the rest of your life. Casey’s story is one of someone who’s really worked hard,” says Dr. Marshall. “She progressed to getting back to the things she loves, to her family, and impressively, back to teaching on a full-time basis, which is pretty remarkable.”
For the latest on Casey’s recovery and to hear her BIG surprise, listen to episode 62 of Pulse Podcast below:
The Ottawa Hospital is a leading academic health, research, and learning hospital proudly affiliated with the University of Ottawa.




