
When someone arrives to The Ottawa Hospital’s intensive care unit (ICU), saving their life is the number one priority. But that’s just the first step. A comprehensive team of physicians, nurses, and allied health professionals team up to help patients not just survive but also thrive. Michelle Cummings plays a critical role in helping make that happen. An ICU physiotherapist at The Ottawa Hospital since 2003, and at our Civic Campus since 2005, Michelle sees some of our most severe and challenging cases. By getting these patients moving as soon as possible, using the latest technology and research to guide her work, Michelle is making sure the worst cases have the best outcomes possible every day.
Keep reading to learn what high school experience inspired Michelle to become a physiotherapist — and why she’s excited to move to the new hospital campus when it opens.
Q: When did you realize you wanted to be a physiotherapist?
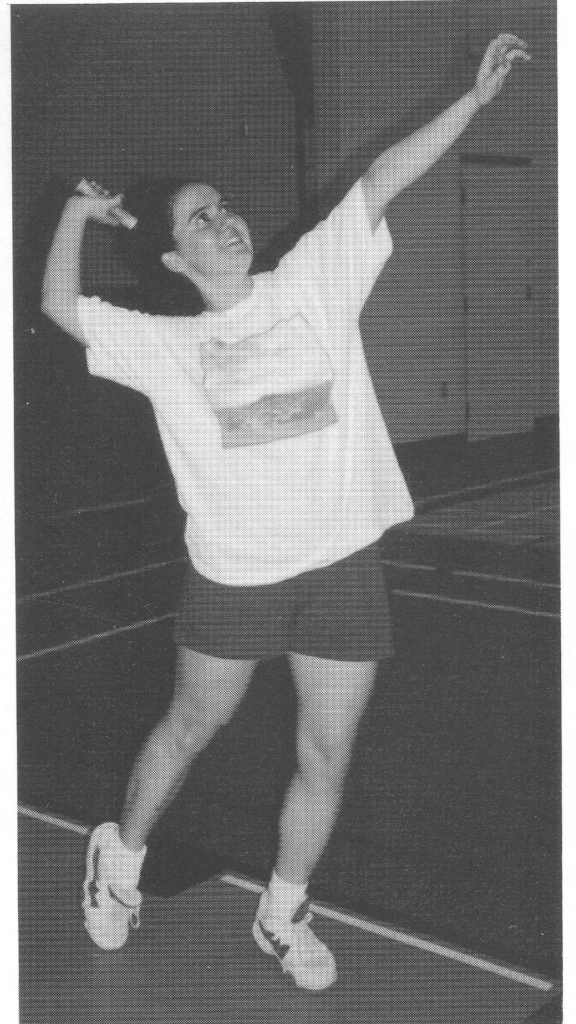
A: I went into physio because I sprained my ankle one too many times in high school. Growing up, I played lots of sports. I was no pro athlete by any means — you’d never see me in the Olympics — I just enjoyed being active. I wound up spraining my ankle three times in six months: first, playing in a badminton tournament — I finished and came in second; next, in an aerobics class in gym; and finally, walking into English class.
My mother had been in a car accident, so she was a big believer in physiotherapy and made me an appointment. At the appointment, the physio and I wound up chatting a lot, so he made a separate appointment for me to come in and talk about how to become a physiotherapist.
Q: How did you wind up working in the ICU?
A: I went to uOttawa for physiotherapy straight out of high school, and at first, I thought I’d work with athletes on sports teams. But during university, I had a placement in an ICU at one of the hospitals in Windsor, close to where I grew up, and my direction in life changed quickly. When I saw that hospital setting, I thought, “This is cool; this is not the type of work I thought we did.”
“I work with patients who are having the worst day of their life, and I get to help them get better.”
— Michelle Cummings
As much as I love sports, I just felt like this fit my personality better. I love working as a team, and in the ICU. If there’s a really sick patient or someone in a bad car accident, the doctors and nurses are going to do their job, and the respiratory therapists, dieticians, the whole the rest of the team will do theirs — everyone is going to work together to get this patient home.

Q: What’s something surprising about the field of physiotherapy?
A: People don’t realize physios work in every area of the hospital. When I tell people what I do, they say, “You work where?!” We work in the ER, ICU, on all the floors, consulting in other departments like obstetrics, with outpatients, and in rehab. It’s quietly connecting everything. We’re part of these teams, and we’re getting people moving and improving strength.
Q: You worked with Aida Attar, a young woman who had a seizure while swimming and had to be revived. What made her case so unique?

A: The thing with Aida is she was very young. And it’s helpful to be young, in terms of recovery. But it was a very serious case. We had to wait until she was awake enough to start physiotherapy, and that was about a month after her accident. We started with two people holding her, sitting on the side of her bed, and she could barely hold her head up. Within a couple weeks, before she left the ICU, she was doing weights and walked a short distance on her own. We have a funny argument about that: she was taking steps with a walker, and I had her walk two metres forward, and I said, “You walked!” and she said, “I just transferred!” She claims I just wanted to be the first one to have her walk, but she really did walk that day!
There were tears and also moments where we laughed over something silly we’d both seen on TV. But she’s a tough cookie, that one. Once she started walking, holy moly, she was so motivated she barely needed me anymore!
Q: You participated in a study called CYCLE (Critical Care Cycling to Improve Lower Extremity Strength). What do you love about research?
A: This study was fun, because we got to use a piece of technology to have patients in the ICU cycling while relatively bedbound and to see whether it improved outcomes. We’re really trying to maintain any function at all in patients who can’t move for long periods. Some patients love it, some hate it, but there’s considerable evidence that early mobility is the best thing we can contribute to a patient’s recovery, to get them moving and in bed cycling can be another great tool to accomplish this with certain patients.
We also are able to use the equipment outside of the study. We had this one patient who had a brain tumour and was not able to walk but was very motivated to get moving. I’d pull out my phone and put on his choice of music — ABBA — and he reached his goal to bike 10 km on it one day before leaving the ICU!

I also complete outcome measures for the SAHaRA. The group has been researching blood transfusions in subarachnoid hemorrhages, bleeding on the surface of the brain, and patient outcomes at six months and one year. As a physio who works with patients experiencing this in the ICU, I don’t always hear how my specific patients are doing after. The research is valuable and reminds me that many people across Canada and the world are surviving brain injuries, regaining function, and getting back to their lives.
I’m a bit of a nerd, and I love reading articles. Any time research comes across my plate, I’ll take it. After 20 years, I still want to find new challenges.
Q: The Ottawa Hospital’s new campus will be the most modern and technologically advanced hospital in Canada. What will that mean for your work?
A: It’s going to be unreal to have the room and the accessibility to do amazing things for our patients. Right now, at the Civic, it can be really hard, because it’s an old campus, the rooms are really small and the equipment is cumbersome. It’s like playing Tetris getting patients out of bed.
The technology will be great, maybe I won’t have to take my phone out to play ABBA, and there will be lifts in every room to facilitate getting out of bed. But accessibility is even better. Can you imagine not being able to easily access the toilet because you just can’t get into the bathroom? In the new campus, that just won’t be a thing.
Q: What would we find you doing when you’re not at work?
A: I have two sons who are 12 and 14, and my two boys along with my husband and dog — a mini aussie doodle — are my biggest priorities. They like gaming, so I game with them. We do lots of walking and camping as a family.
If I’m not with my first or second family — my work family — I’m with my third one: my taekwondo family. I’m frequently there, not spraining my ankle (so far). There’s nothing more therapeutic than striking an inanimate object over and over again!




