Published: August 2024
Like many university students, Erin Brown, a kinesiology undergrad at uOttawa, was burning the candle at both ends. When she started to complain about headaches, nausea, and seeing stars, those close to her believed she was pushing herself too hard. Even her doctor initially said, ‘You need to take a break’. But as symptoms worsened, Erin soon learned it wasn’t stress or exhaustion; she had a brain tumour — and it was a type the world hadn’t seen before.
The 21-year-old was in her fifth year of her undergrad in human kinetics studies in 2018 when the symptoms started. When they worsened, she paid another visit to her family doctor who did some neurological tests, but couldn’t pinpoint the cause. “He said if the symptoms continued, I should go to the nearest emergency room and get some imaging done,” explains Erin.
It wasn’t long before her dad took her to an area hospital, and after initial tests, Erin was sent to the Civic Campus of The Ottawa Hospital. Dr. Safraz Mohammed, a neurosurgeon specializing in brain and spine, was on call when Erin arrived at the Emergency Department.
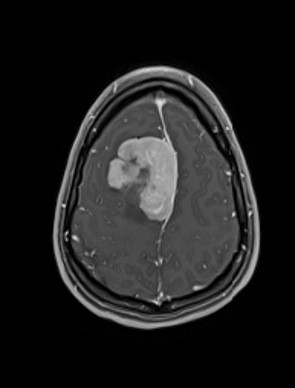
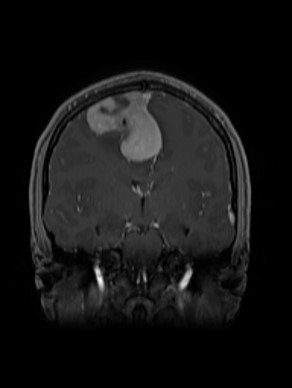
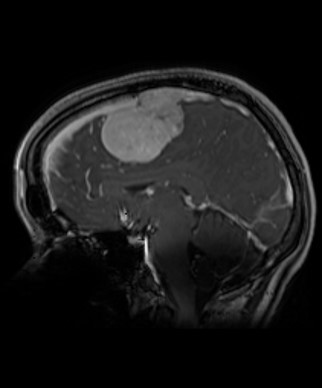
“After reviewing her CT scan, we immediately ordered an MRI scan, and that unfortunately revealed a brain tumour in her right frontal lobe,” says Dr. Mohammed.
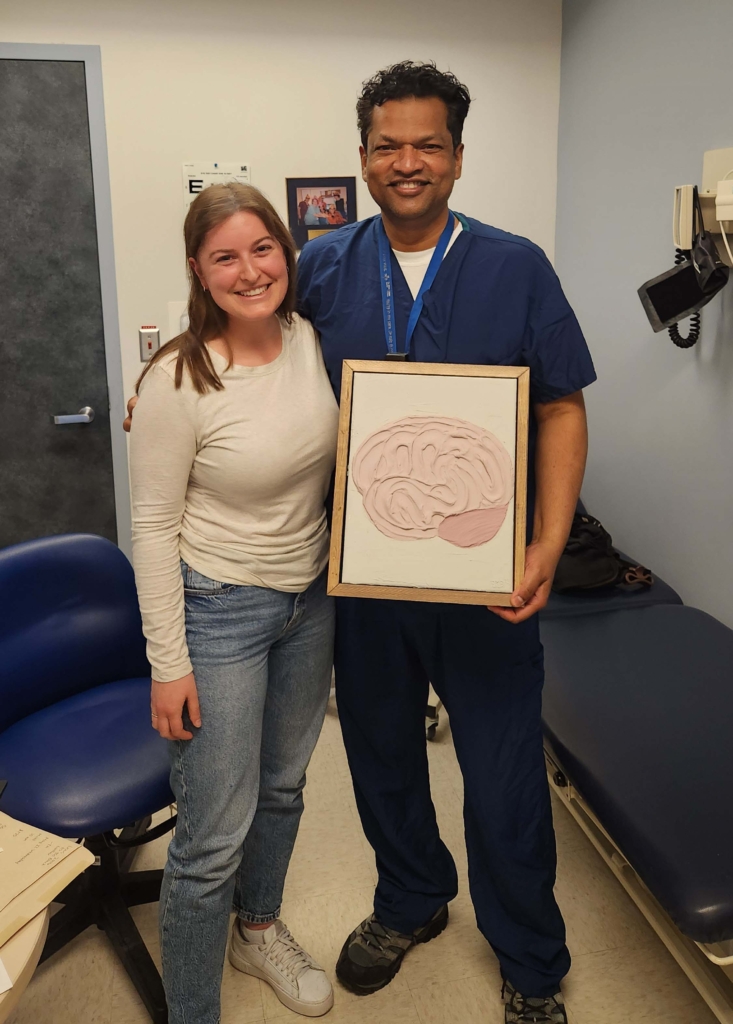
He remembers those early interactions with Erin quite well. “She had such an uplifting spirit, even at the time of diagnosis. I could see that she was an amazing person and she was going to be a great patient.”
For Erin, the feeling is quite mutual. This young doctor, just two years into his career, brought her much ease. She was admitted to F7 (the neurosciences inpatient floor) and had another MRI the next morning. When Dr. Mohammed came to meet with Erin and her family — he sat down.
“When I meet patients, I sit down at the eye level. I sit on the bed sometimes or sit on a chair close to them, because I think it’s important to be at eye level to have good patient interaction rather than having a height difference.”
He also jokes that it’s a good opportunity to sit down after operating all day or being on rounds.
A type of tumour never seen before
Erin’s tumour was quite large — the size of a small apple — and all signs indicated it was a meningioma, which is a type of tumour that develops from the membrane that covers the brain and spinal cord. In Erin’s case, it was invading the middle vein in the brain known as the superior sagittal sinus, which is a major vein and damage to it can result in devastating consequences, according to Dr. Mohammed.
“Those devastating consequences include a massive stroke, massive bleed into the brain, and unfortunately, even death. It’s a big vessel, but it has a thin wall. It would take a lot of planning for the surgery.”
After careful planning, Erin was prepped for surgery with Dr. Mohammed and his team. A continuous trans-esophageal echocardiogram was used to ensure that no air was sucked in through the main vein, as this could result in death. Dr Mohammed wanted to remove the entire tumour, given that Erin was so young. During the six-hour procedure, the tumour was completely extracted and sent for analysis.
"That’s when we discovered this tumour had elements to it that were never seen or discovered before."
— Dr. Safraz Mohammed
The testing yielded the most unusual results. Dr. Mohammed learned it was a grade 3 tumour, which meant it was cancerous. “It wasn’t benign, as we suspected. It also didn’t follow the criteria for meningioma. As a result, we sent it for further testing in Toronto, and that’s when we discovered this tumour had elements to it that were never seen or discovered before,” explains Dr. Mohammed.
This new type of tumour is called a dural-based spindle cell neoplasm, characterized by a novel MN1-KMT2A fusion gene, based on the type of cells and genetics discovered within it. This tumor was unlike anything ever seen or described before. With the neuropathologist’s help, the team was able to publish this new tumour in the medical journals.
It was difficult news for Erin to grasp. “I remember becoming so overwhelmed with emotions that I just started crying. This is a lot more serious than I thought, but Dr. Mohammed calmed me down. The nurse in the room, Nancy Mongeon, was so sweet and nice,” explains Erin.
“My parents gathered themselves too, and then we just talked about next steps. I was never scared after that because of all the reassurance I got — I just knew I was in good hands, and I just had to trust my team,” adds Erin.
Ready for treatment
Because the team was working with a new type of tumour, there was no precedent for treatment. But since they knew they were dealing with a grade 3 tumour, they recognized radiation was required.
That’s when Dr. Vimoj Nair, a radiation oncologist who specializes in the treatment of children and young adults, stepped into the picture. He brings a particular skill and knowledge in high-precision radiation therapy, including his work with the CyberKnife — a radiosurgery robot that can destroy inoperable brain tumours, as well tumours in other parts of the body. This important piece of equipment was acquired thanks to donors of The Ottawa Hospital.
“We are proud to have access to cutting-edge technology here at The Ottawa Hospital and of our decades of experience when it comes to radiation treatment.”
— Dr. Vimoj Nair
It was Dr. Nair and his research collaborators who first published the made-in-Ottawa platinum seeds used to improve an already incredibly powerful and precise radiosurgery treatment system for tumours in the liver, pancreas, and kidneys. “We are proud to have access to cutting-edge technology here at The Ottawa Hospital and of our decades of experience when it comes to radiation treatment,” explains Dr. Nair.
As Erin was so young, Dr. Nair wanted to give her the best chance at a full life, without recurrence. “It’s not just giving radiation, but there’s ensuring the patient can have good survivorship and maintain all their capacities. She’s young, and we wanted a plan to spare her memory centre, so she has full use of her brain.”
That meant targeting the tumour, but also covering the area around the tumour to treat any potential microscopic disease that human eyes or scans cannot detect. “It’s like a tree on the lawn. You can cut it down, but you still must go after the roots of the tree,” he explains. “This meant using the linear accelerator machine, which could give a lower dose per day to a wider area and allow normal irradiated brain tissue recover, instead of using the CyberKnife, where an intense radiation treatment is given to only any visible tumour.”
By late 2018, after 30 rounds of radiation, the team was hopeful.

Becoming a part of TOH family
It was during those weeks of radiation treatment that a switch flipped for Erin. It had nothing to do with her health, but rather her career aspirations. Dr. Mohammed remembers when Erin shared this part of her journey. “She talked to me about how she was so much younger than the other patients around her and how much compassion she had for the older people who were also having radiation. She started helping them up, helping them move across the room, and getting paperwork or whatever it was they needed.”
This proved to be a defining experience in her life — a spark in her journey towards healthcare.
Dr. Mohammed could see what an exceptional nurse she would make, and he was there to support her. “I wrote her a reference letter for nursing school and then her training led her to Sunnybrook Hospital in Toronto — that’s where I trained during my residency. When her program was wrapping up, I encouraged her to come to work at the Civic because it’s simply the best place to work.”
In 2021, Erin became a nurse in neurology on F7 — the same floor where she was first admitted to when her care journey began three years earlier. The neurosurgical patient became the neurosurgical nurse.

New lesion appears in a different location
As Erin’s career blossomed, she continued regular MRI scans every six months. Then in May 2022, a tiny dot on the right temporal lobe appeared in a scan.
“I discussed it at the tumour board. This is a group of neurosurgeons, radiation oncologists, and neuropathologists from our hospital who discuss complex cases. I wasn’t ready to put her through another operation just yet, so we watched this new lesion closely,” says Dr. Mohammed.
Then two months later, the lesion grew quite a bit, to the size of a grape. By October 2022, Dr. Mohammed and his team returned to the operating room with Erin to perform a right-sided craniotomy in the temporal region, along the side of her head. “This is a new, small tumour in a different location. The original tumour was gone and all the images that we’ve had so far show that nothing grew back there. So, we removed the lesion and as much dura layer or the covering of the brain as I could.”

The way it was described to Erin is this new lesion was the result of a drop metastasis — where a small cell from the original tumour dropped down the side and developed into a new tumour.
Unfortunately, just over a year later, the lesion was back, and in January 2024, Erin faced a third surgery to fully resect it, followed by more radiation. Consensus from the tumour board was radiation helped long term with the first tumour, so they should proceed with radiation on the second one.
This time, the challenge was to treat the brain in a different location but minimize overlap with the previous radiation plan, ensuring a good balance between tumour control and any short-term and long-term toxicity risks in a young patient.
“At TOH we are proud to have access to cutting-edge technology and an experienced radiation planning and therapy team. We’re able to spare the brain and it shows our expertise in treating younger brains,” explains Dr. Nair.
Focused on a career of caring
Today, Erin continues to be monitored closely and more treatments lie ahead but she also takes what she’s learned as a patient to the bedside when caring for her patients — knowing firsthand what they are going through.
“It’s such a privilege to take care of patients when they’re in their most vulnerable state, knowing the degree of what they’re going through even though each experience is different.”
— Erin Brown
She has a special connection to those younger neuro patients with whom Erin can relate. “I’ve had a couple of younger patients who were in their 30s and 40s. They just look so scared. They’re going home to their family. They have young kids. They don’t know how to navigate it, and I feel for them because I’ve kind of been in their situation. Maybe not 100%, but I know to a degree what they’re going through, so I’m able to give them that support.”
As for the unprecedented tumour that put her in the history books, she jokingly wishes they had called it an “Erinoma”. Regardless of what her future holds, she’s grateful for the highly skilled team who brought not only their expertise, but also a sense of calm during the most challenging time in her life — a team she was proud to be a part of. Today, Erin is working in the ICU at the Cornwall Community Hospital.




