All about strep A
What exactly is strep A?
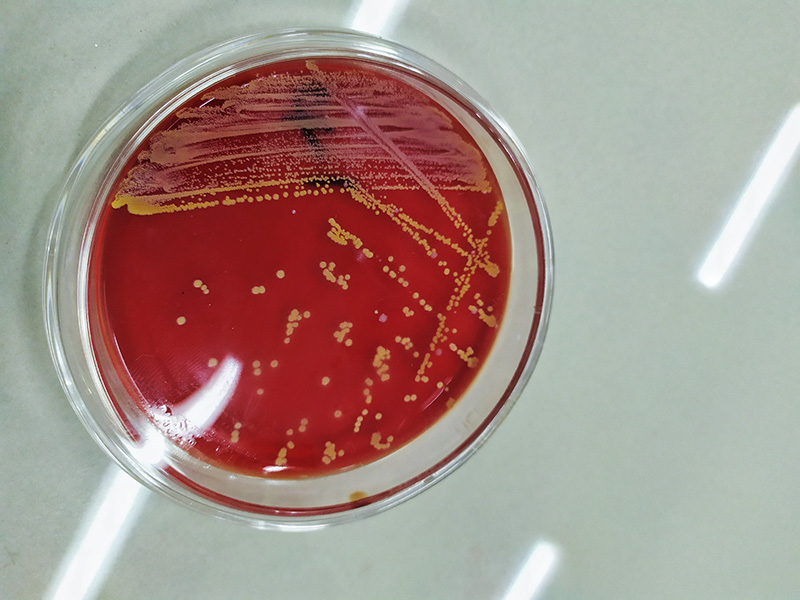
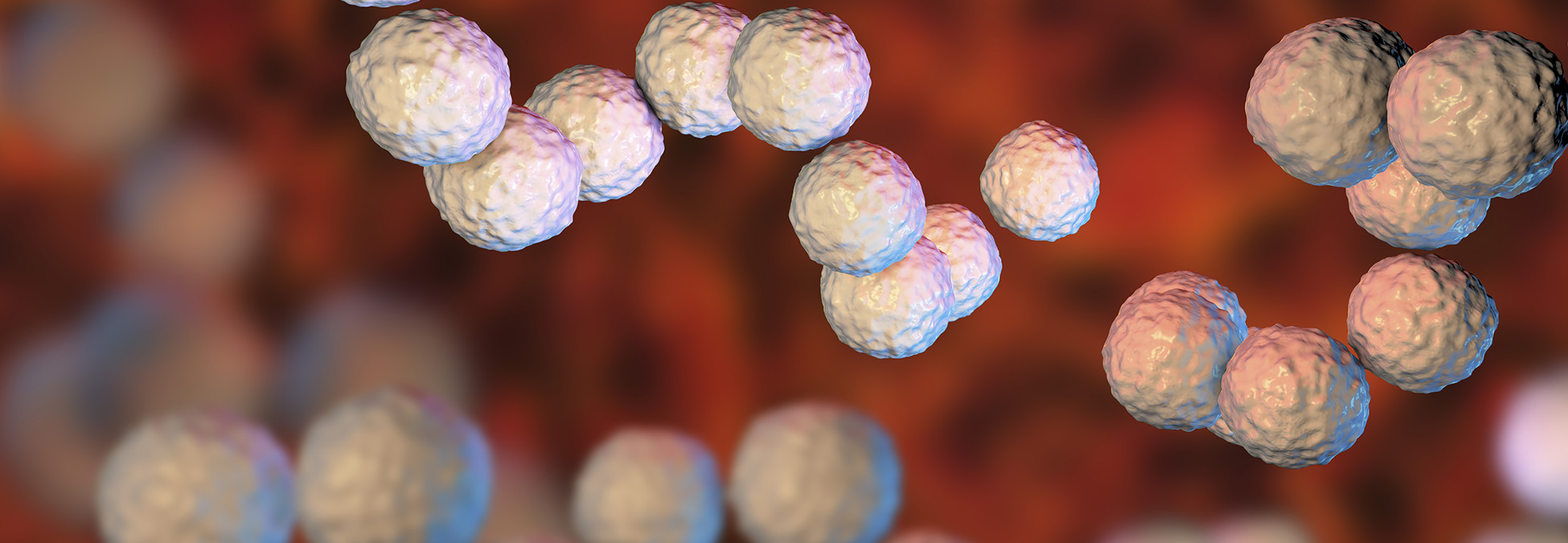
Strep A, full name group A streptococcus or streptococcus pyogenes, is part of the larger streptococcus genus of bacteria. In 1877, Viennese surgeon Albert Theodor Billroth named streptococcus from the Latin words strepto (twisted) and cocco (berry), because the bacteria looks like a twisted chain of spheres under a microscope.
Strep A is often found as part of the normal skin, throat, vaginal, or anal flora. Usually, there are no signs that strep A is present.
Strep A infection pushes photographer Sean Sisk’s life to the brink
What is a group A streptococcal infection?
The vast majority of strep A infections are mild or moderate, occurring where the bacteria is found. These are called non-invasive strep A, and they’re diseases like strep throat, impetigo or wound infections, and scarlet fever.
On the other hand are the more invasive strep A infections, when the bacteria migrates to a part of the body where it’s not usually found. These infections can become serious and life-threatening very quickly.
Strep A is a contagious bacteria that usually spreads through respiratory droplets or direct contact with infected skin.
Long-term issues related to strep A infections can also emerge — such as post-streptococcal glomerulonephritis and rheumatic fever — which are caused by the body’s immune system response to the infection itself.
People who are immune compromised — due to illness, injury, medication, age, or other causes — are at a higher risk of contracting a strep A infection.
How are strep A infections treated?
For non-invasive strep A infections, usually a round of antibiotics is enough to take care of the infection.
For invasive strep A infections, hospitalization with antibiotics is usually required. If it has caused necrotizing fasciitis, surgery is often required to prevent the spread of the disease.
What is the future of strep A?
Cases of invasive strep A have been rising for years, with rates in Canada approximately doubling between from 2.7 to 5.6 cases per 100,000 people between 2001 and 2021. It’s hard to pinpoint the exact cause, but experts point to everything from increased international travel to increases in people using shelters and long-term care facilities to COVID-19 weakening people’s immune systems.
Despite attempts beginning in the 1930s, there is currently no vaccine for strep A. For now, prevention remains a major priority. Prevention can include taking antibiotics prophylactically if you’ve had close contact with someone with a severe case of invasive strep A infection, washing hands after coughing and sneezing or before eating, and keeping wounds clean and watching for signs of infection, such as redness, swelling, pain, or fever.