Published: November 2025
Read time: 2:30 mins
Published: November 2025
Read time: 2:30 mins
Tracy Bacenas is all too familiar with storytelling. She’s been an editor for widely popular TV reality series, such as Survivor, Amazing Race, and The Bachelor, where she’s kept viewers on the edge of their seats. For years, she thrived in the fast-paced world of Los Angeles before trading in the palm trees for Canada’s capital, where she moved with her Canadian husband 15 years ago and where they welcomed twin boys.
However, nothing in her career prepared her for her own story that was unfolding — a diagnosis of a rare bone cancer. She quickly learned about the access to specialized care at The Ottawa Hospital — something for which she would later develop a deep appreciation.
Shocking news of a rare cancer
While Tracy worked remotely from Ottawa, she stayed active, playing sports with her sons, running, and walking many kilometers daily to get away from the constant screen time that comes with her work.
In 2023, she started having hip pain that she attributed to autoimmune issues she’s had over the years. “Then I started limping because it started to hurt badly. My family doctor initially thought it might be bursitis, so she sent me for an X-ray,” says Tracy.
“At the bottom of the report it read ‘chondrosarcoma can’t be ruled out’. I froze. And I had this really bad feeling in the pit of my stomach.”
— Tracy Bacenas
As family tried to reassure her everything would be okay, Tracy and her husband, Jason, met with the orthopaedic oncology team at The Ottawa Hospital and confirmed Tracy’s fears. “Tracy had chondrosarcoma, a malignant bone tumour of the pelvis and it also involved the hip joint. These tumours can spread and metastasize — they’re dangerous tumours,” explains Dr. Joel Werier, Head of The Ottawa Hospital Sarcoma Program and orthopaedic oncologist.

Chondrosarcoma is a rare type of cancer that usually begins in the bones, such as the pelvis, hip, and shoulders, but can sometimes occur in the surrounding soft tissue. Most chondrosarcomas grow slowly and may not cause many signs and symptoms at first. Some rare types grow rapidly and have a high risk of spreading to other areas of the body, which can make these cancers difficult to treat.
Limited treatment options for chondrosarcoma
Dr. Werier explained to Tracy that surgery was her only option for this type of cancer. “It’s very important that we remove the full tumour, but the challenge is it meant removing a good portion of the pelvis and the hip joint, so mobility becomes an issue.”
This was devastating news for Tracy. “How do you hear that? My life was active. My vacations, especially with my sister, were all around hiking and going to walking cities with my husband. It was a rough, rough day.”
However, thanks to medical advancements, The Ottawa Hospital can offer some patients a new option for bone reconstruction — a 3D customized pelvic implant.

New medical innovation in a 3D custom implant
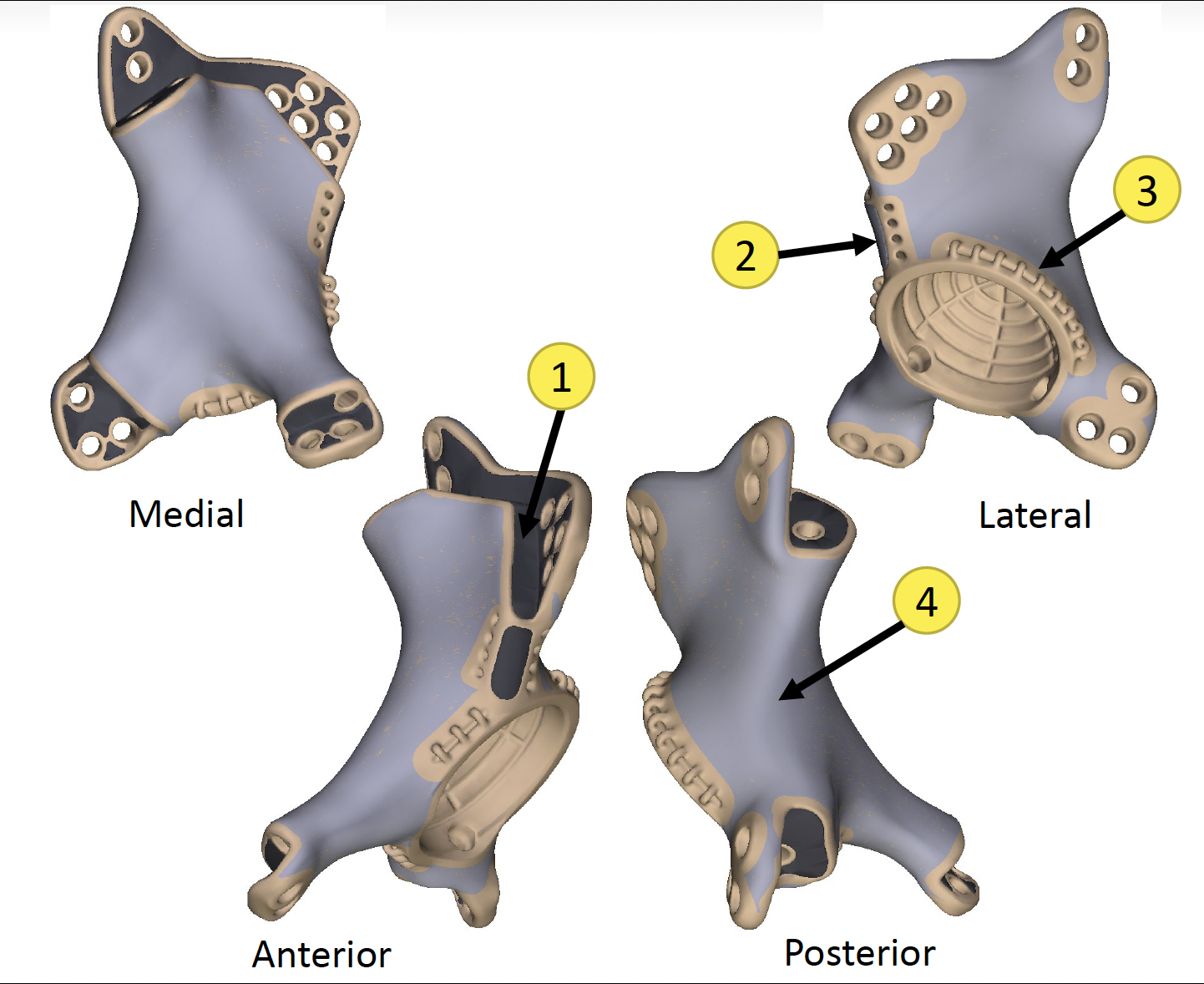
The 3D pelvic implant is custom designed based on MRIs, CT scans, and other imaging. It is silver coated to reduce the risk of infection — a risk associated with this option.
That’s where Dr. Hesham Abdelbary comes in. He’s an orthopaedic oncology surgeon, who was a part of Tracy’s surgical team, and he’s also focused much of his research on associated implant infections. “We’re looking at how we deal with this problem. If someone is cured from their cancer but then they must deal with an infection, outcomes can be unfavourable. I hope our research can improve care for this complex problem,” explains Dr. Abdelbary.
Complex orthopaedic surgery planned
The 16-hour operation was set for February 2024, and once the tumour was removed, the surgical team placed the implant. “The design comes with guides to make sure the prothesis fits, and Tracy’s fit perfectly to her bone. It recreated the pelvis that was removed, and you have a hip replacement, as opposed to an empty hip,” explains Dr. Werier.
The implant is made with a porous type of metal, which over the course of 12+ months allows the surrounding bone to grow into the implant, giving the patient a solid pelvis.
The surgery was a success and Tracy spent six-weeks in hospital. She credits her family, including her husband, her sister, and many friends for their support in helping her through this difficult time. She also is grateful to the hospital team that surrounded her during those weeks.
“You’d think I would have been bored because I couldn’t move, but I was never bored. There was a constant flow of nurses and staff — they were all so kind,” explains Tracy. “There was Miller, who helped bathe me and washed my hair. Just a beautiful soul with healing vibes. The lady who came in to clean the room treated me like a person, not just another patient in the bed. And still to this day, when I’m at the hospital, I run into Renée, the porter who brightened my long days in rehab.”
It was how the care team treated her like family that left a lasting impact. Tracy points to nurse Ali, who was by her side immediately after surgery and continued to check in on her. “She sang to me, held my hand when I cried, hugged me, and gave me pep talks when I needed them most.” And during the weeks that followed, nurses like Shukharat Akinwande, an orthopedic surgery nurse, made sure Tracy was well-cared for and getting stronger each day.

Learning to move with a pelvic implant
“I felt like I had so many people in my corner, making sure I had the best outcome possible.”
— Tracy Bacenas
Tracy’s next stage of recovery was at The Ottawa Hospital Rehabilitation Centre, where she met another dedicated group, whose sole focus was to get Tracy moving again. From Dr. Trudel, who led her care team, to Alison Davis, her physiotherapist, to Frankie Nadeau, her occupational therapist, and Sanja Schlumberger, who identified swelling in her leg was the result of lymphedema, and many more, Tracy is deeply grateful. “I felt like I had so many people in my corner, making sure I had the best outcome possible.”

Frankie recalls when Tracy arrived, she was using a wheelchair almost exclusively. They started slowly with a goal of getting her back home where she could function more independently. “We focused on standing tolerance and confidence, so building her strength back up.”
The pair really hit it off and Tracy recalls their laughter could be heard through the halls. Frankie is known as a real-life “MacGyver”, of sorts, for her ingenious solutions for patients. “She introduced me to the sock aid — that was huge. That helped me put my socks on myself. It gave me my first taste of “new normal” independence,” recalls Tracy.
After a month of intensive rehab, Tracy was ready to go home. “By that time, I was riding a hand-cranked bicycle around the courtyard outside of rehab. I went from barely being able to stand up to walking with two crutches.” she says.
Grateful for specialized, modern medication close to home
Today, the two-time Emmy nominated film and television editor, continues her road to recovery. Tracy returned to editing but also teaches at Algonquin College’s film program.
She is scanned every three months and meets with Dr. Werier. She continues her physiotherapy, and swimming has become a big part of rehabilitation. Her mobility continues to improve, but she still uses a wheelchair for longer outings.
Despite some challenges, she finds comfort in her surroundings. As someone who was born in the United States and lived there much of her life, she’s grateful this happened while she was living in Ottawa.
"Having this type of care here for people in Ottawa and people close to Ottawa, and having a doctor like Dr. Werier here — holy smokes, how lucky are we?”
— Tracy Bacenas
“I’m so thankful because if I had to go to Toronto or Vancouver, or to the States, I can’t imagine the expense, and being alone would have been awful. If I had been living in the US, it would have bankrupted me. So, having this type of care here for people in Ottawa and people close to Ottawa, and having a doctor like Dr. Werier here — holy smokes, how lucky are we?”
As for Dr. Werier, he credits this type of innovative technology for giving patients a new quality of life and hopes to see it continue to improve and advance to expand to other patients in the future. “This is a huge advancement. We’ve used it in several other situations. It’s a very powerful technology.”






