Stefanie Scrivens vividly remembers the first time she experienced a mini-seizure, though she didn’t know what it was at the time. She was only 13 years old, but her symptoms continued undiagnosed for nearly a decade, until a CT scan revealed Stefanie had a brain tumour that would become cancerous if untreated. Her best chance of survival was undergoing two 8-hour awake brain surgeries, performed by neurosurgeon Dr. John Sinclair, and a highly skilled team of experts at our hospital.
Frightening symptoms
Stefanie was in elementary school, walking to class, when she noticed a metallic smell and taste in her mouth, followed by blurred vision. These strange symptoms only lasted a few moments, but afterwards she was disoriented, confused, and struck with a severe headache. “I’m just tired,” Stefanie thought, and went on with her day as if nothing happened. But these symptoms continued, up to 20 times a day, for a week straight, every six weeks — a frightening experience for anyone, let alone a teenager.
Stefanie’s parents were concerned and brought her to her family doctor. “I was told they were growing pains. That I was just going through puberty. I thought what I was going through was normal,” said Stefanie. But as her symptoms progressed year after year, she would eventually discover it was anything but normal.
“Dr. Seale didn’t just chalk it up to anxiety or say that I would grow out of it. He was willing and ready to help me figure out what was going on.”
— Stefanie Scrivens
A twist of fate
When Stefanie was 20 years old, new symptoms developed. That’s when she decided to pay a visit to the Emergency Department (ED). She needed to get to the bottom of the symptoms she had experienced for nearly half of her life. This is where she met Dr. Edward Seale, who was one of the attending physicians at the ED.
It was a twist of fate that Stefanie landed in Dr. Seale’s examination room that day. Dr. Seale immediately recognized her symptoms as mini-seizures. “As someone who has epilepsy myself, seizures and the symptoms one may experience while having one, were top of mind for me,” said Dr. Seale. “Although each physician here would have treated her the same way, seizures are a part of my life, so I could relate to what she was going through.”
Stefanie was relieved to finally feel heard. “It felt like for the first time in my life, someone actually understood what I was going through,” said Stefanie. “Dr. Seale didn’t just chalk it up to anxiety or say that I would grow out of it. He was willing and ready to help me figure out what was going on.”
Due to the repetitive nature of her symptoms, Dr. Seale thought she may have epilepsy and ordered her a CT scan to investigate further. But the results from her scan turned out to be far worse than Stefanie could have imagined.
A shocking diagnosis
When Stefanie’s results came in, Dr. Lucian Sitwell, a Neurologist at The Ottawa Hospital broke the news. The cause of her mini-seizures was a grade 2 oligodendroglioma, which is a type of slow-growing brain tumour that becomes cancerous. “Until that moment, the thought had never crossed my mind that it could be a brain tumour,” said Stefanie. As she sat there shocked and scared, she cried. At only 20 years old, this news was devastating.
But a few moments later, she made a crucial decision. Stefanie decided to stay strong, positive, and do whatever it took to fight for her life. “I was of course upset, but I thought to myself ‘I have a choice right now. I can either be angry this is happening to me, or, I can try to make the most of it.’ And I decided, worse comes to worse, if I don’t make it, I don’t want to leave this life with a negative mindset.”

After absorbing the difficult news of her diagnosis and learning what her treatment options were, Stefanie, armed with her “ready to tackle anything” attitude, decided to move forward with treatment, which would include a complex, 8-hour awake brain surgery.
An innovative treatment plan
Stefanie was referred to Dr. John Sinclair, a world-class Neurosurgeon at The Ottawa Hospital, who would be in charge of her treatment plan and surgery to remove the tumour. Dr. Sinclair has been at the forefront of bringing new and innovative treatment options and technology to The Ottawa Hospital, such as the CyberKnife, Advanced Awake brain tumour surgery, and most recently Fluorescence Guided Surgery. This has brought new hope to patients with unique brain tumours, like Stefanie.
“I felt that I could trust putting my life in his hands.”
— Stefanie Scrivens

“Stefanie’s case was rare,” said Dr. Sinclair. “It isn’t very often that you see healthy, young individuals, like Stefanie, with a diagnosis like this.” Fortunately, global advances in cancer research at the time indicated a new treatment plan for tumours such as oligodendroglioma was showing promising results. And Stefanie was a good candidate for this new treatment. “Over a decade ago this wasn’t common practice. We would have monitored the tumour and once it started to change we would recommend surgery then radiation and chemotherapy as a form of treatment,” explained Dr. Sinclair. “Now, we’re seeing a significant increase in life span and survival rates, in cases such as Stefanie’s, when we surgically remove the tumour as soon as it’s detected. No longer are we using radiation and chemotherapy as a primary treatment method for this type of tumour.”
After meeting Dr. Sinclair, Stefanie had full confidence in her healthcare team “Going under the knife is really nerve racking. But not only did I hear how great Dr. Sinclair was as a neurosurgeon, I realized after meeting him how great he is as a person, too,” said Stefanie. “He took the time to get to know me and develop a good relationship with my family and me. I felt that I could trust putting my life in his hands.”
Stefanie was fortunate to benefit from having the tumour surgically removed before it turned malignant. And after a successful complex 8-hour awake brain surgery, she was back home recovering just three days later.
Awake brain surgery and brain mapping
Awake brain surgery, used to treat some brain tumours such as Stefanie’s oligodendroglioma, is a type of procedure performed while a patient is alert and communicating normally while in the operating room. Brain tumours are often dangerously close to regions in the brain that control vision, speech, cognition, personality, and movement. By keeping a patient awake during surgery, they can monitor a patient’s brain activity throughout the procedure to ensure they aren’t negatively impacting these important functions. “Tumours are often woven with functional tissue,” explained Dr. Sinclair. “In the last five years we’ve been able to use more advanced brain mapping techniques so that we can more accurately remove the tumour without hurting the patient.”

Subcortical mapping is a very new technique used in brain mapping surgery — and our experts are some of the first to use it and are leading the way in training others. As an expert in the field, Dr. Sinclair and his team have offered courses to physicians from across the country so that they too can make use of this revolutionary technique that is changing the lives of patients, just like Stefanie.
Back to the operating room
Within three weeks of her awake brain surgery, Stefanie was back in school. Determined to become a doctor herself one day, she didn’t want to miss a semester of pre-med courses. But after a few months, she felt her symptoms were returning. “I was starting to feel really tired and I was getting seizures again,” said Stefanie. Knowing this could be a part of the healing process, Stefanie wasn’t concerned. But when it was time for her checkup, MRI scans showed scar tissue and the possibility that the tumour had returned.

Stefanie would need to undergo a second awake surgery to remove more tissue from her brain. But she wasn’t going to let this get in the way of her dreams. “I thought I would have my surgery, take a bit of time off school and then head right back to my studies,” she said. Dr. Sinclair was able to remove both the scar tissue and some areas concerning for tumour progression. By all accounts, the surgery was considered a success. But while in recovery something significant and unexpected had changed for Stefanie. “I woke up thinking all I wanted to do was bake.”
Becoming a Michelin star pastry chef

Le Cordon Blue Ottawa Culinary Arts in 2012.
For a year straight following her surgery, Stefanie baked a cake every day. “It was so meditative and healing for me,” Stefanie said. She knew medical school was no longer the right path for her. She had new dreams — to become a professional baker.
In 2012, she graduated from Le Cordon Blue Ottawa Culinary Arts Institute and went on to work for some of the top Michelin star restaurants in the world — a career that has been fulfilling on many levels.
When Stefanie decided to undergo treatment, she didn’t anticipate the experience would change the course of her life so dramatically. She credits The Ottawa Hospital for giving her the chance to chase her dreams and explore whatever the future might hold for her. “Thanks to my incredible healthcare team I’ve lived my life to the fullest and I don’t take any day for granted,” said Stefanie. “I’ve been able to check everything off my bucket list and now I’m writing a new one, with even more dreams to chase.”
Hope for the future
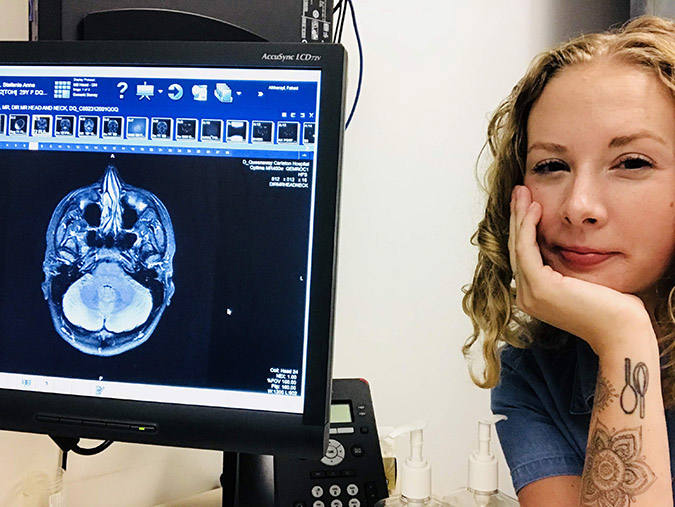
At first glance, you would never know Stefanie went through full-day awake brain surgeries — her blonde, curly hair covering any remaining scars she has accrued. She’s a strong woman who hasn’t let any negative circumstance in life get her down.
“With this new treatment method for oligodendroglioma, I can’t say that a cure is impossible.”
— Dr. John Sinclair

The innovative treatment, which removed the tumour before it could become cancerous, meant Stefanie has been able to indefinitely postpone both chemotherapy and radiation. Under the care of our experts, Stefanie is feeling better than ever. Her latest scans show there is no sign of recurrence.
“Stefanie is in unchartered territory,” said Dr. Sinclair. “We can’t say for certain if or when the tumour will come back. But, with this new treatment method for oligodendroglioma, I can’t say that a cure is impossible.”
Because of the excellent care Stefanie has received at our hospital, she has decided to continue to live near Ottawa. “My hope is to continue to be looked after by this group of incredible doctors,” Stefanie said. “I feel so fortunate to be in their care.”
Listen to Episode 88 of Pulse Podcast to find out how Stefanie’s doing today and why she’s excited about the new campus development.
The Ottawa Hospital is a leading academic health, research, and learning hospital proudly affiliated with the University of Ottawa.




