
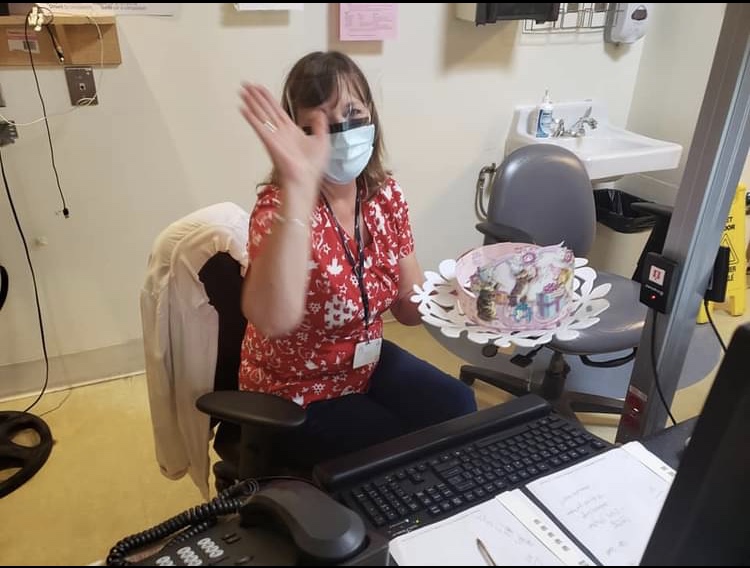
For many people, visits to the hospital are few and far between. But for others, trips to the hospital are much more regular. This is certainly the case for the patients with kidney disease that nurse Robin Laird works with at The Ottawa Hospital’s Riverside Campus Nephrology Clinic. Having worked in the unit for more than 30 years, Robin is a familiar face for the patients who have to come in up to three times a week for dialysis, and she plays a critical role not only in patients physical health, but also in their emotional health.
Whether she’s caring for someone who’s been receiving treatment for decades or someone who’s coming in for the first time after a sudden illness, Robin’s compassion drives her care every day.
Keep reading to learn more about why Robin chose to work in nephrology and some unusual facts about kidney disease.
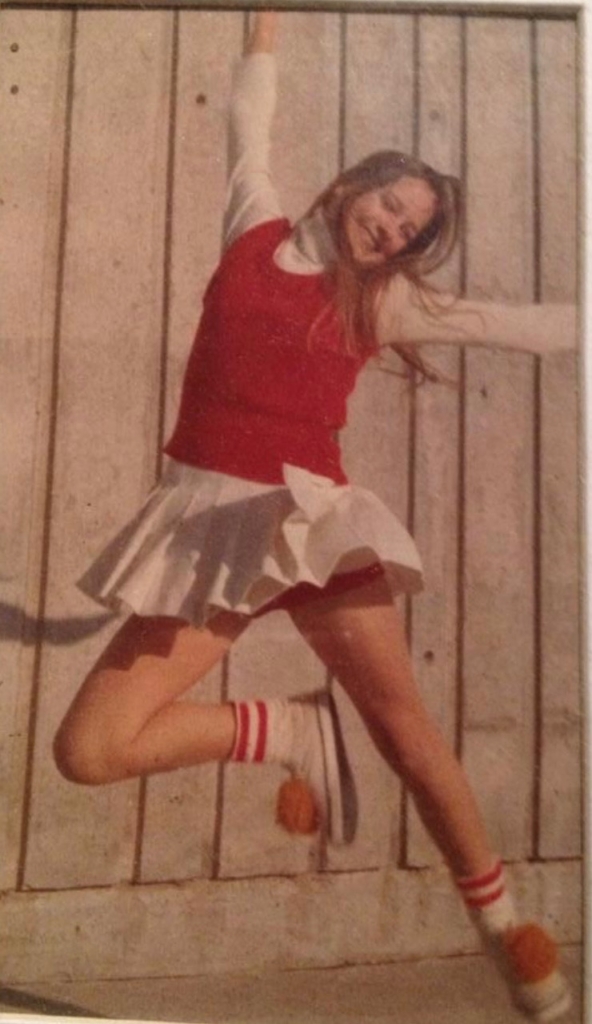
Q: Can you tell us a little bit about your childhood and early years?
A: I grew up in Belleville and I was a teenager of the ’70s — I was a cheerleader, on student council, and I loved high school. I married my high school boyfriend, and we’re still married. In school, I loved English and history. The sciences were OK, but it depended on who the teacher was. I did a lot of babysitting; I loved little kids.

Q: When did you decide to become a nurse — and specifically in nephrology?
A: There really wasn’t anything else I was ever interested in. It’s funny, when I went into nursing, I thought I would like to be in the delivery room, but I soon found it wasn’t for me. I worked for the Trenton Hospital for five years on the medical floor then moved to Ottawa in 1986 and put in an application at the Civic. I got a phone call shortly after asking if I was interested in nephrology. In college, nephrology hadn’t come up that much, but once I got into it, it was the perfect fit — I’ve never looked back. I think I’m one of the longest working nephrology nurses in the program at The Ottawa Hospital now!
Back working on the medical floor, there was always a sense that you could never quite fit everything into a day. But working in dialysis, you do your duty, you make your patient feel better, and they leave at the end of the day. You get a sense that you’ve accomplished your day.
Q: What is something unusual or surprising about nephrology and dialysis?
A: The most surprising thing is that some people with kidney disease look perfectly healthy — you’d never know they’re sick, yet they’re at risk of death if they don’t have dialysis. Another thing people might not understand is that once you’ve started dialysis, you can’t just opt out of it.
Another surprising thing is that when your kidneys don’t work, you don’t make urine — you don’t pee. Some have very residual renal function and have a little urine output, but many don’t. Any fluid just stays in your blood. We have to do a calculation to remove the fluid for them during dialysis.
I have to teach my patients that while others might think carrying around a great big water bottle is healthy, for these patients, it’s not – they have to stop that.
So when patients come in with their extra-large double doubles — which can be up to 500 mL — I just say, “We’re going to have to go down to a small, extra small, because the fluid restriction is only one litre a day!”
Q: You were one of the nurses in Katie Skidmore’s case. What made that case so unique?
A: We have two kinds of patients that come in: those who have had kidney issues for years and eventually decide to go on dialysis and those who have acute kidney failure and have no time to prepare.
Katie came to us with this sudden, life-altering diagnosis of anti-glomerular basement membrane (anti-GBM) disease in her 30s. She was a young woman who’s living a big, healthy life, and suddenly she’s given this blow. At this stage, patients are often in a stage of grief, so it was important to help her with the physical and medical aspects, but also emotionally.
Katie is also so smart that nothing escaped her. She would watch things like her blood values: when her antibodies went down, it meant she was recovering, but when that didn’t happen, she would crash. She’s unique in seeking out her results and in being proactive.
I’m so proud of Katie and how far she’s come. I saw her in the unit the other day, and she was on the phone, laughing and talking. It’s such a leap for her.
Q: If someone has just been diagnosed with kidney disease, what advice would you give them?
A: I think the biggest thing is that kidney disease doesn’t necessarily mean the end of your life — it’s just a chapter; don’t jump to the end of the book. And, you’re not alone. The program we have at The Ottawa Hospital is amazing in the support we have for patients. I’ve seen it over the years since 1986, and the whole thing is exceptional. You have choices, and you can decide your journey.
Q: What keeps you motivated during stressful times as a nurse at The Ottawa Hospital?
A: Two things: colleague support and realizing you get a break from this.
Nursing is a stressful job, but we come together as a team. The support we get from each other in the lunchroom cannot be underestimated. My best friends are all from the nephrology program, we call each other sisters, and many of us have been working together over 30 years.
No matter how stressful it is for me, I also have holidays. My patients never get a holiday. If they’re lucky, they can go somewhere, but they still have to do their dialysis.
Q: What would we find you doing when you aren’t at the hospital?
A: I live in the country with my husband and two adult daughters and a cat. Before COVID, I was a big-time party planner and did all the retirement planning for the nurses. I love home décor — thrifting, flower arranging. I’m also in a book club with retired nephrology staff, and there are 13 of us. We’re very strict about it and put out questions. We kept it going through COVID and just started in-person ones again in the summertime.



