As a young boy, Cody Church was constantly asking his parents the same dreaded question, over and over again, “why?” But everything changed in high school when he discovered physics and suddenly felt like every “why” he’d ever asked finally had an answer — and now he could find it.
Today, a medical physicist at The Ottawa Hospital, Cody is applying his passion for finding answers to developing the best ways to treat patients receiving radiation. Using the latest technologies to personalize treatment, Cody is improving patients’ experiences and outcomes every day.
Find out why Cody Church chose The Ottawa Hospital and what he’d be doing if he wasn’t helping patients.
Q: Can you tell us a bit about your early years?
A: I grew up in Dartmouth, Nova Scotia with a sports-heavy upbringing. I played hockey, baseball, and basketball, even if I was too short to play that last one well. As a teenager, I started my addiction to golf, and I just wish I’d started earlier.
From about 15 onwards, I held three part-time jobs pretty consistently: I started as an umpire in baseball, and then I worked as a dishwasher, at a grocery store, and at our local events centre. I started as the kid walking up and down the steps with popcorn and worked my way up to the guy walking up and down with beer and eventually working the bar.


Q: What was your favourite subject in school?
A: In elementary school, I loved math. Then, in high school, I found physics, and it was like the blinders had been removed. I was a big “why” kid, which is what makes any curious kid hard to parent. With physics, it’s the study of “why” at its most fundamental. Suddenly, I was getting answers to every question I’d ever had.
Q: What did you want to be when you grew up?
A: As with most academically keen kids, I thought I might become a doctor. I did all my course selections, volunteering, etc. to do a program at Dalhousie University that would prepare me to go down the medical school route. Once I was in the program, though, I realized being a doctor wasn’t for me. The level of memorization didn’t appeal, and I wanted to be doing more problem-solving.
Q: What was your path to medical physics?
A: I switched into physics after my first year, but I didn’t find medical physics until my fourth year of undergrad. To work as a medical physicist in Canada, you almost always have to have a PhD, so I did my master’s and PhD at Dalhousie in health and medical physics.
Q: What exactly is medical physics?
A: Medical physics refers to physics in and around how it might be used within the human imaging and therapy domain. There are four flavours of medical physicist, and about 85% are in radiation oncology, like me. We are concerned with the safe use of radiation for therapy and imaging. Other types of medical physicists are those concerned with using electromagnetic radiation in MRIs; those who work with nuclear medicine; and those who work exclusively with diagnostic imaging (ultrasound and mammography, etc.), who are pretty rare.
Q: Why did you choose to come to The Ottawa Hospital?
A: Things are so darn competitive that you have to do a two-year residency to work in medical physics. I applied to multiple places, and I made my decision to come here because I was looking for people I’d want as colleagues, and the interview in Ottawa was the closest I found to an East Coast experience in terms of the warm reception.


Q: What’s something that surprised you about working in medical physics?
A: What really surprised me about the field was the importance of multidisciplinary interpersonal relationships in actually translating things into clinical utility. You spend so much time in school learning about fundamental physics, the ABCs of being a physicist, but when you start a job, there’s a certain status quo about how things are done. There can be serious inertia. I wouldn’t have been able to get the newest device I’m using out there if I hadn’t developed good relationships with both ends of our radiotherapy workflow, which allowed it to happen very fast.
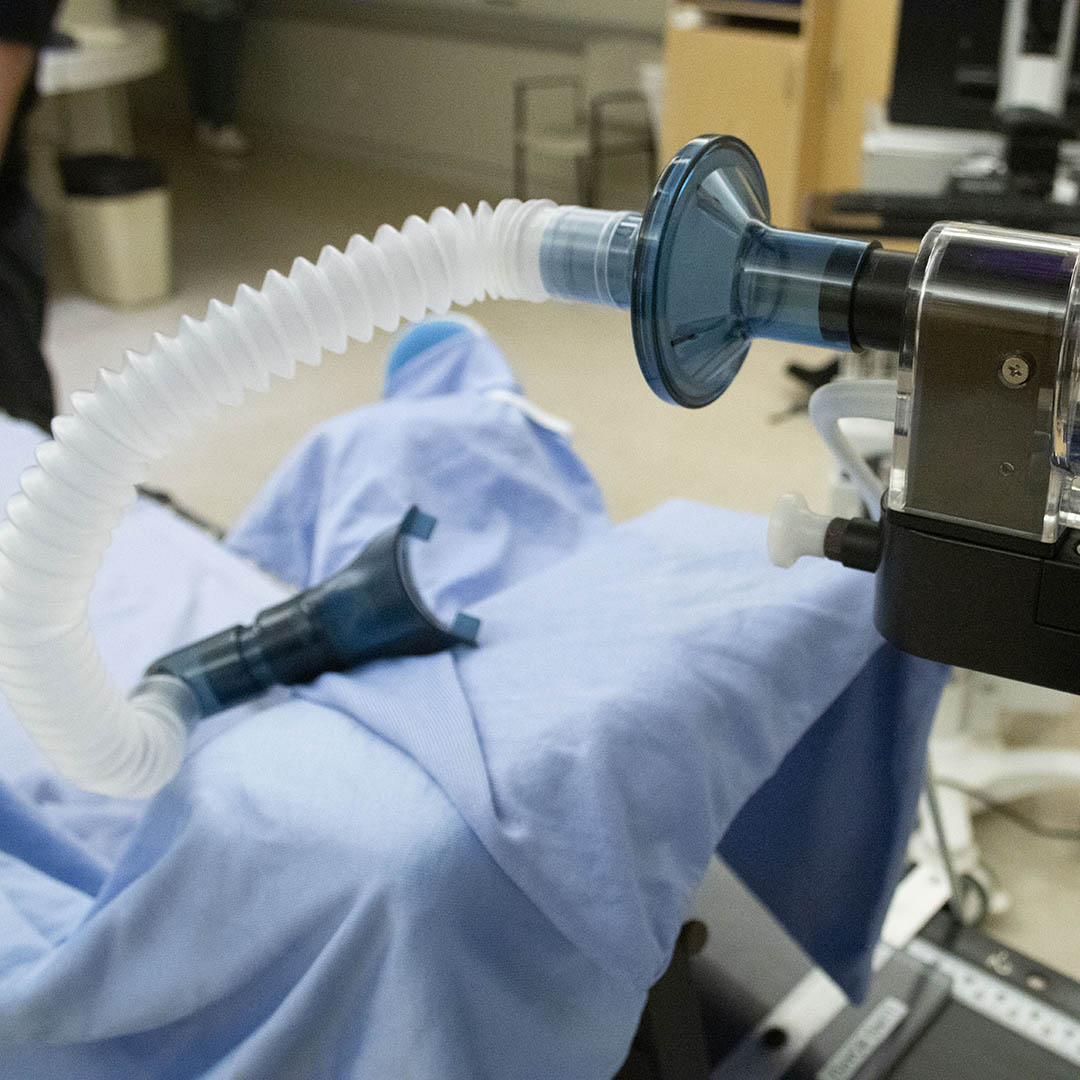
Q: Can you tell us about this new device, the active breathing coordinator?
A: We treat patients with a machine that rotates around them, delivering very small amounts of targeted radiation. We try and find a clear path for delivery, and respirations, or breathing, can cause patients’ organs to move while they receive treatment.
The active breathing coordinator (ABC) measures the amount of air patients breathe into their lungs and is then used to hold their breath for them so we can treat them very precisely. The ABC allows us to be more accurate and precise when we pinpoint our radiation doses, potentially reducing side effects and long-term risks.
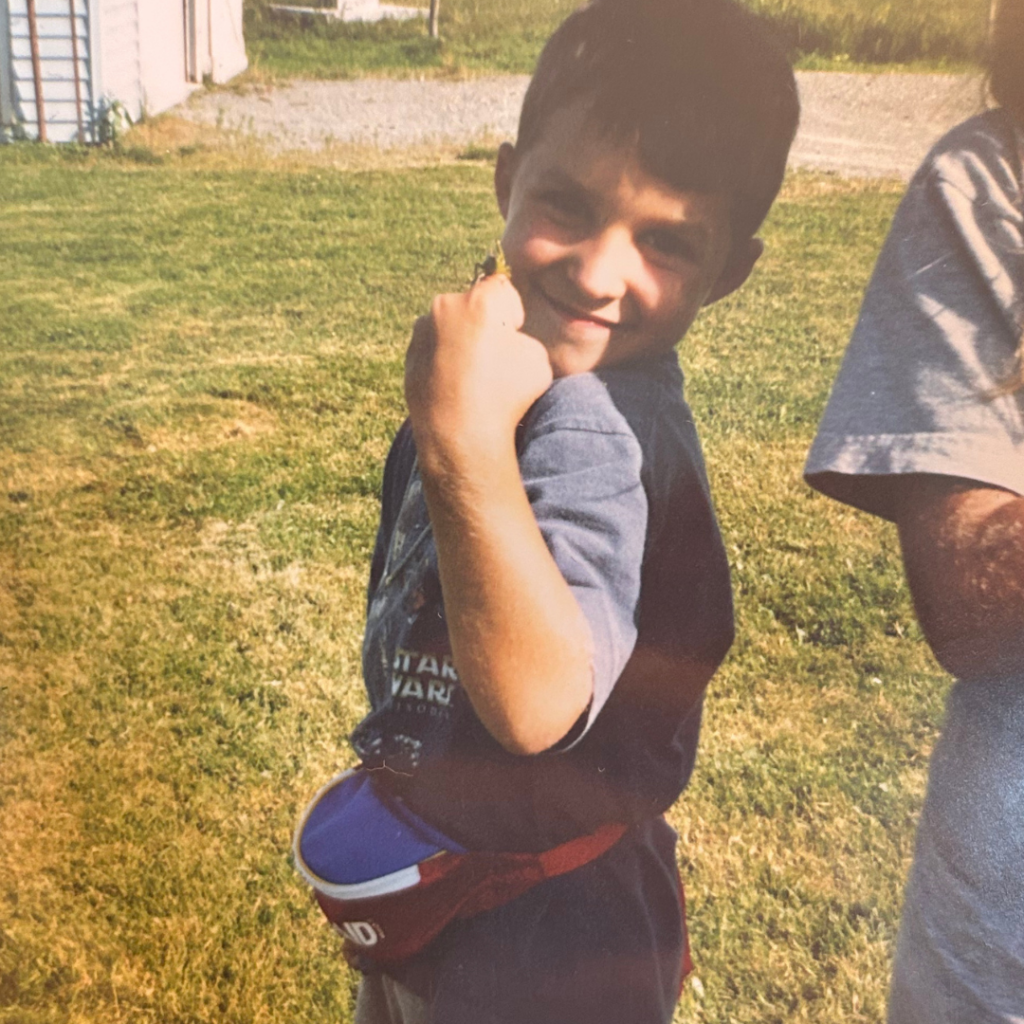
Recently, we treated a pediatric cancer patient with the ABC for the first time in Canada. We have to screen patients very carefully to see if it’s appropriate for them, and a young patient came in who had an excellent understanding of his capacity and abilities, and we were able to treat him with the ABC.
Q: How is The Ottawa Hospital pushing the boundaries of radiation therapy?
A: A hot term in radiation therapy is adaptive radiation therapy, which means changing the treatment plan during treatment based on changes in the patient. The Ottawa Hospital recently installed a state-of-the-art MR-Linac machine, a hybrid machine that uses magnetic resonance imaging (MRI) and radiation therapy, which enables us to see tumours during treatment and adjust our therapy in real-time.
We’re one of the first centres in Canada to have an MR-Linac machine, and we’ve only treated a few people with it, but the ability to make on-the-fly changes that are personalized to give the most optimized treatment on the very day of treatment is the future.
Q: How does having access to the new technologies help your patients?
“”Having access to new technologies provides options. Every person who comes in for treatment is unique and deserves personalized therapy. “
— Cody Church
A: Having access to new technologies provides options. Every person who comes in for treatment is unique and deserves personalized therapy. Having a multitude of different options allows us to pair different technologies to give the most optimal treatment.
As a medical physicist, I’m biased, and we like to have a lot of toys, but it’s truly about giving everyone the best chance through the best care.
Q: What career do you think you’d pursue if you weren’t a medical physicist?
A: As a detail-oriented perfectionist, I’d probably be a cook or a barista. Right now, I have a love/hate relationship with cooking because of how much time it takes, but I love all the aspects of fine dining.
Q: Where would we find you when you’re not at work?
A: You might find me making coffee; I have my process dialled in and all the good tools, like a calibrated tamper, but that only takes about five to 10 minutes. The rest of the time, you might find me with my husky. I got her when I was 20, at the peak of my undergraduate degree, and there’s a lot of outdoor time, although not as much now that she’s 11. I still play hockey and golf, and I play beach volleyball with a couple of pals. We get crushed, but it’s still fun. And I read a lot of fantasy!