Published: August 2025
Read time: 3-4 mins
Published: August 2025
Read time: 3-4 mins
- Our hospital has a specialized clinic that supports pediatric cancer survivors through their adult years, for those facing long-term effects of cancer treatment.
- An innovative combination of technologies to treat a tumour located near the heart of a young patient with lymphoma was a first in Canada for this type of pediatric case.
- The goal is to deliver an exact dose of radiation to the cancerous tumour, targeting malignant cells to destroy or shrink them, without affecting the healthy cells.
For young patients facing cancer, every milimetre matters — radiation treatment must be delivered with extreme precision to make every effort to avoid damaging the healthy, and sometimes still growing, surrounding tissue. Thankfully, The Ottawa Hospital is a leader in this field, providing care for all residents in Eastern Ontario, Western Quebec, and Nunavut, including children. Recently, our hospital took a big step forward to give patients a better chance at a full recovery with fewer side effects from radiation. For younger patients, who are still growing and have a full life ahead of them, this is critical progress.
It is estimated that about 50% of patients diagnosed with cancer will need to receive radiation treatment during their cancer journey — either as a stand-alone treatment or in combination with chemotherapy and/or surgery. While the Children’s Hospital of Eastern Ontario (CHEO) remains the primary treatment center for pediatric cancer in our region, radiation treatments for young patients are administered at The Ottawa Hospital. This collaboration ensures that children and their families receive the most comprehensive care available.
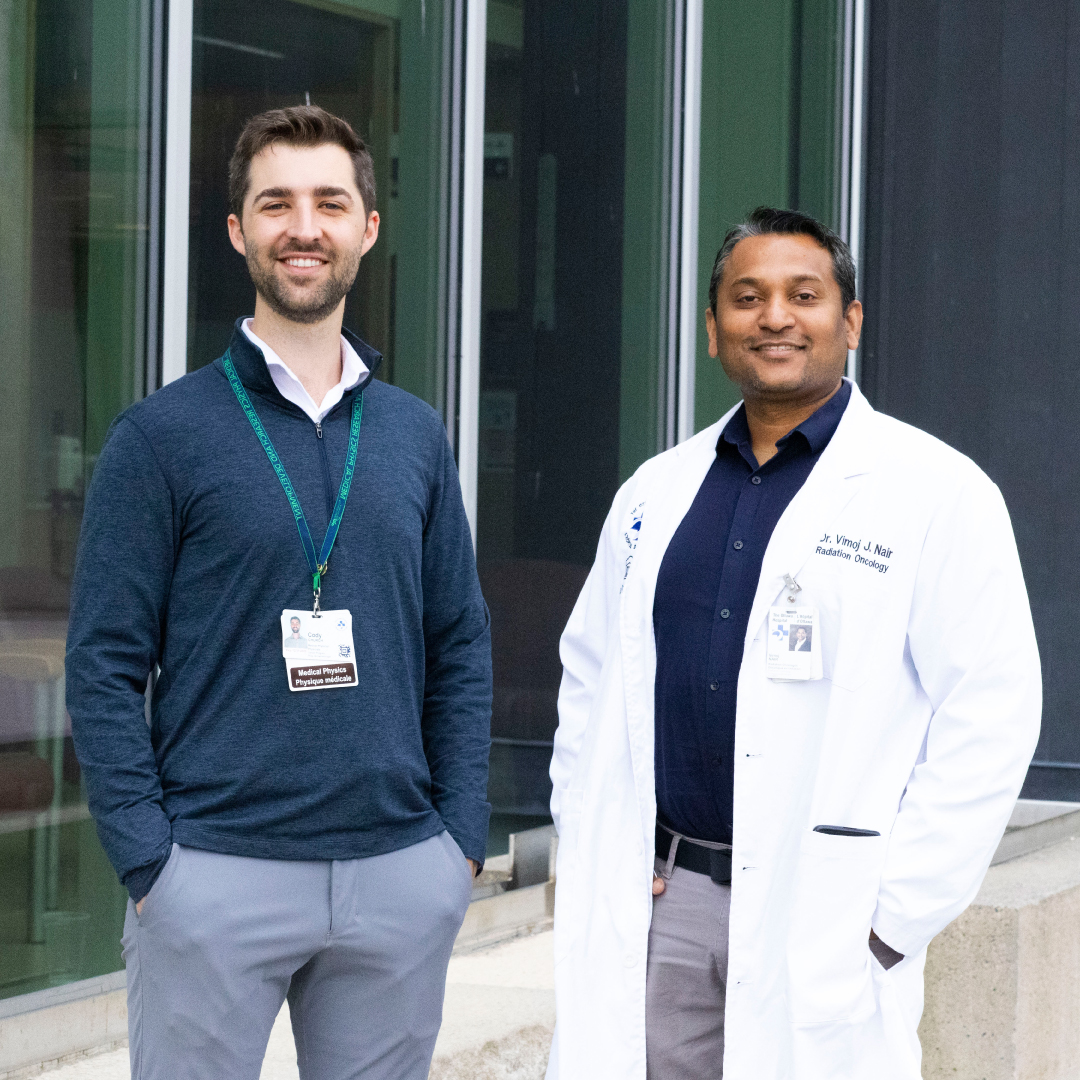
Meet radiation oncologist Dr. Vimoj Nair
Supporting pediatric cancer survivors into their adult years
Dr. Vimoj Nair, a radiation oncologist, is one of two specialists at our hospital who specialize in the treatment of children and young adults with cancer. He explains why the precision of radiation is vitally important to avoid serious complication from the treatment, later in life. “When a young patient goes into remission and they turn 18, they graduate from CHEO. As many as 80% of childhood cancer survivors will develop a serious or life-threatening late effect by age 45. As a result, they need a lifetime of monitoring, and that’s where we come in.”
This form of long-term follow-up care comes from a program known as the Pediatric Oncology Group of Ontario (POGO) clinic. It’s a specialized clinic that supports pediatric cancer survivors through their adult years, and our hospital provides this support for those facing long-term effects of cancer treatment.
Hodgkin’s lymphoma is an example of a cancer that impacts teenagers and has a high chance of remission. Radiation is often a part of the treatment plan.
Supporting pediatric cancer survivors into their adult years
For young patients facing cancer, every milimetre matters — radiation treatment must be delivered with extreme precision to make every effort to avoid damaging the healthy, and sometimes still growing, surrounding tissue. Thankfully, The Ottawa Hospital is a leader in this field, providing care for all residents in Eastern Ontario, Western Quebec, and Nunavut, including children. Recently, our hospital took a big step forward to give patients a better chance at a full recovery with fewer side effects from radiation. For younger patients, who are still growing and have a full life ahead of them, this is critical progress.
It is estimated that about 50% of patients diagnosed with cancer will need to receive radiation treatment during their cancer journey — either as a stand-alone treatment or in combination with chemotherapy and/or surgery. While the Children’s Hospital of Eastern Ontario (CHEO) remains the primary treatment center for pediatric cancer in our region, radiation treatments for young patients are administered at The Ottawa Hospital. This collaboration ensures that children and their families receive the most comprehensive care available.
Meet radiation oncologist Dr. Vimoj Nair
“This type of cancer usually occurs in the chest around the heart. While radiation successfully cures the cancer in more than 90% of patients, it can also inadvertently expose the adjacent heart to moderate doses of radiation, increasing the long-term risk of heart disease or failure,” explains Dr. Nair. “At the POGO clinic, monitoring is done for such late effects — we’re talking for 20 or more years into the future. So, our team is always on the lookout for new technology to reduce such late side effects from therapy in young patients and pediatric patients who have long survival chances.”
New treatment provides the lowest dose of radiation
Our team of specialized radiation experts is constantly looking for new ways to ensure the best outcome for our patients — long term. Thinking outside the box, they used an innovative combination of technologies to treat a tumour located near the heart of a young patient with lymphoma — a first in Canada for this type of pediatric case.
While similar approaches may have been used in adult patients, the use in pediatric patients remains extremely rare. “This technique was perfected at The Ottawa Hospital for this type of patient. It significantly reduced radiation exposure to the heart and lungs, offering meaningful protection against long-term side effects — an especially important consideration for such a young patient,” says Dr. Nair.
Imagine being able to keep a patient’s body so still, not even a small breath could alter the intended target. Cody Church is a medical physicist at our hospital. Along with his team of colleagues, including Kim Charbonneau, he led the implementation of a device called the active breathing coordinator (ABC).
Meet medical physicist Cody Church
“The device communicates with our machines to turn the radiation beam on and off based upon a threshold that we set,” explains Cody. “We calibrate the device to each patient’s comfort level so that when they inhale to that point, the device will hold their breath and the radiation beam will turn on. When the hold-breath hold is over, the beam is paused, allowing the patient to regain comfort before the next breath-hold.”
Older models of the ABC required the therapist to manually turn the beam on and off, making treatments longer and precise targeting more difficult.
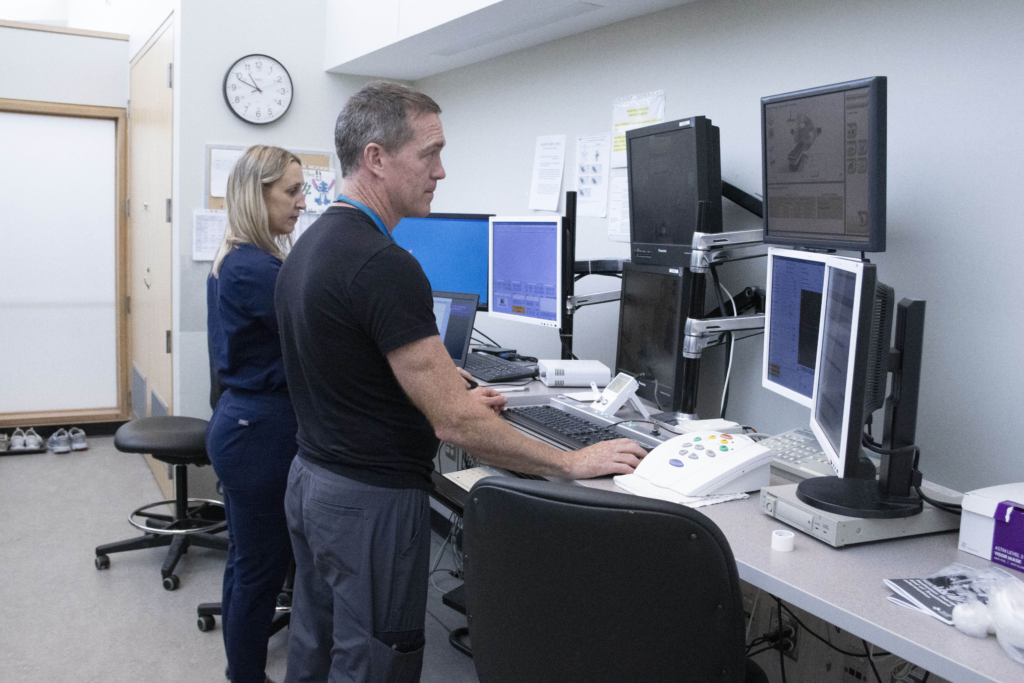
“With standard technology, radiation is delivered while the patient breathes, which means everything within the radiation field — both the tumour and surrounding areas like the heart — can be irradiated. Since breathing causes the heart and other organs to move, this results in less precise treatment,” explains Dr. Nair. “With this new technique, we stop that motion by having the patient hold their breath during the radiation. This ensures the treatment is delivered only to the tumour, allowing for far more accurate and targeted radiation with least dose to the surrounding healthy tissues and hence less late toxicities in this young person.”
Meet medical radiation therapist Kim Charbonneau
How this innovative technique works
The goal is to deliver an exact dose of radiation to the cancerous tumour, targeting malignant cells to destroy or shrink them, without affecting the surrounding normal cells. This accuracy helps limit the side effects for the patient.
The ABC device has a small plastic mouthpiece, similar to that of a snorkel, that sits on the patient’s teeth. A bendable arm is connected which controls the software that monitors breathing. It’s a process the patient practices many times to prepare for this moment.
“The idea of the device is to have precise control of the breath-hold volume so that we accurately reproduce the position of the tumour and surrounding healthy tissue every time. It might sound extreme to have a machine controlling your breathing for you, and the first time you experience it, it’s a little shocking, but after you understand what the feeling is like, you get it right away,” explains Cody.


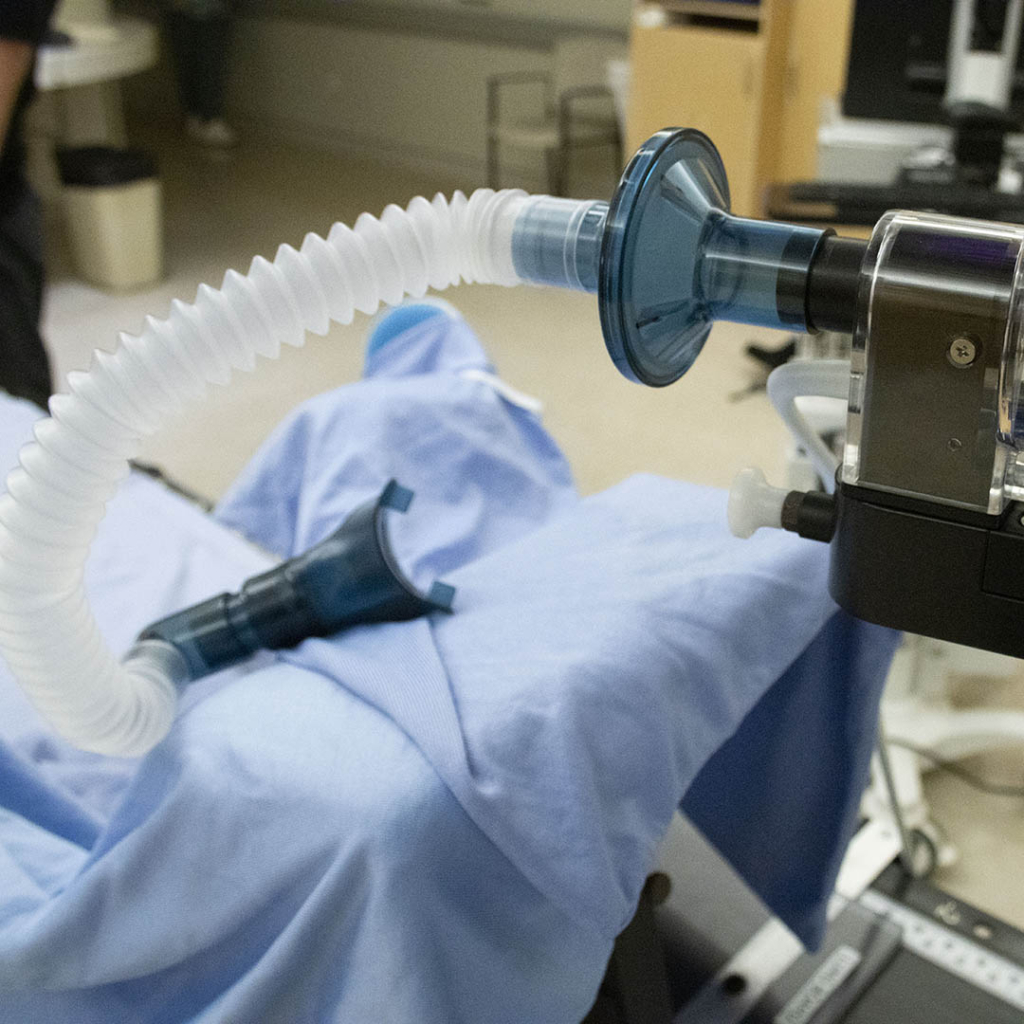
This treatment was delivered by the patient inhaling for 30 seconds, known as an inspired treatment. While it can also be delivered through exhaling, there are more benefits when the patient inhales. “There’s a reason why we like the inhalation a bit better for this treatment because the heart will push down and away when your lungs fill up with air, moving it away from the intended target.”
On average, the patient would repeat this process between nine and 15 times during one radiation treatment.
If at any point they feel like they can’t proceed or keep up, the care reverts to the original standard treatment plan to ensure they get the best outcome possible.
Giving young patients in remission the best chance at a long, healthy life
This new option, especially for young patients, brings fresh hope for a long, healthy life. “This is the best surrogacy for what’s happening inside the body during treatment compared to other technologies that are available. Usually, these are things like markers on the chest to monitor as a patient breathes, or some optical camera shining on the chest looking at the skin. All have pros and cons, but with the ABC, we are measuring what’s happening inside,” explains Cody.
It’s important to note, this type of radiation treatment is not for everyone. It depends on a patient’s capabilities — adults or teenagers — the details of their case, and making sure there is constant coaching and preparation. But the team is excited to be able to offer it as an option now, especially to young patients.
“It’s the most efficient delivery possible and pediatric patients are the ones who benefit the most, so it just seemed like the perfect marriage in terms of applying it in a first group,” says Cody. “It’s an honour to be a part of something that helps patients. I feel like every incremental improvement we can bring for our patients deserves our full effort.”
- Our hospital has a specialized clinic that supports pediatric cancer survivors through their adult years, for those facing long-term effects of cancer treatment.
- An innovative combination of technologies to treat a tumour located near the heart of a young patient with lymphoma was a first in Canada for this type of pediatric case.
- The goal is to deliver an exact dose of radiation to the cancerous tumour, targeting malignant cells to destroy or shrink them, without affecting the healthy cells.




