Published: September 2025
Read time: 2 mins
Published: September 2025
Read time: 2 mins
Dave Hale had a humble upbringing. He grew up in Munster, a small, farm-influenced community in southwest Ottawa. In that quiet environment, much of what Dave learned about life came through the example set by his parents.
His mother, in particular, shaped his understanding of community and service. A special needs educator by profession, she also ran a daycare, taught piano, volunteered through her church, and gave her time to anyone who needed it. Even outside of work, she would step in to support families — offering to care for children with special needs so their parents could enjoy a rare night out. These weren’t grand gestures, but they meant everything to the people she helped.
It was probably the most powerful life experience we’ve ever had. It made me realize that it’s the little, micro things you do over a lifetime that truly matter. You have to ask yourself: What are we really doing with our time here?"
— Dave Hale

“When she passed at age 61, we received over 300 letters from people she had impacted,” Dave recalls. “It was probably the most powerful life experience we’ve ever had. It made us realize that it’s the little, micro things you do over a lifetime that truly matter. You have to ask yourself: What are we really doing with our time here?”
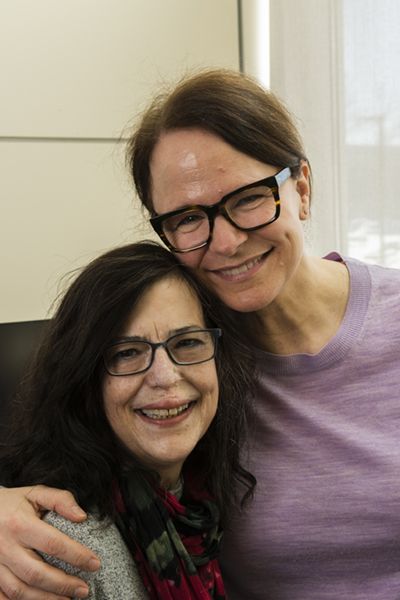
Dave and his wife, Arielle, didn’t learn the value of community through wealth — but by witnessing Dave’s mother’s quiet, selfless acts of service. Now, as parents and business owners, they see how deeply those lessons are shaping their own values. Real impact doesn’t have to be loud, it just has to be intentional and the Hales are determined to create a legacy of service and purpose.

“You can be successful through nothing more than commitment and hard work.”
That mindset has driven Dave from the very start. At just 13 years old, he spent his summers and each autumn working at Saunders Farm, becoming a full-time employee at 17 and the marketing lead at just 20. This experience would set the tone for the rest of his career. Spending those formative years working at Saunders Farm, he watched a small, family-run attraction evolve into a thriving, multi-generational business. That experience didn’t just fuel his work ethic, but it ignited a passion for entrepreneurship.

Through that education and the real-world experience of founding his first business in 2010, Dave began to notice a pattern in how most organizations approached marketing: too much focus on flash, not enough focus on strategy.
In 2025, Arielle and Dave founded RDEL Group — named after his mother’s middle name, Ardell. Built on a “business-first” approach, RDEL Group helps clients grow by spending smarter, through efficient software, streamlined processes, and growth-oriented business development strategies.
The company’s philosophy mirrors the values their family learned from Dave’s mother: that small, consistent, intentional actions can make a lasting impact. Intentional effort, when executed correctly, can drive major results.
Building what matters
Today, Dave is stepping up in his own way as a dedicated volunteer for the Campaign to Create Tomorrow. He, Arielle, and their daughters, Elliotte (7) and Cordelia (6), are making their most significant philanthropic gift yet — one they hope will inspire other young families to think differently about philanthropy and about investing in themselves.
“When you drive down Preston Street, I feel like the future is being built,” Dave says. “It’s not just about tomorrow. It’s about 20 to 30 years from now, for me and my family.”
“When you drive down Preston Street, I feel like the future is being built. It’s not just about tomorrow. It’s about 20 to 30 years from now, for me and my family.”
— Dave Hale
Dave and Arielle want to be a voice for the next generation — asking bold questions about how we give, where our funding goes, and why transparency matters. Because when they visit the new hospital site, they are able to point to the construction and say to their children, we’re helping build that.
“I think it’s an exciting time,” Dave explains. “You can load your kids in the back of the car, drive yourself to Carling and Preston, and show them where your investment is going. That kind of visibility is invaluable for teaching young children.”
For the Hales, making a gift to the new hospital isn’t just charitable. It’s a smart business move. It’s an investment with exponential return: better care for their family, a stronger healthcare system for the community, and a lasting legacy for future generations.
That’s what sets this moment in time apart. The new hospital isn’t just solving today’s challenges — it’s planning for what healthcare in this city can and should be decades from now.
That long-term vision is rare, and it’s exactly what inspires leaders like the Hales to step up and be part of something that lasts.