Published: February 2026
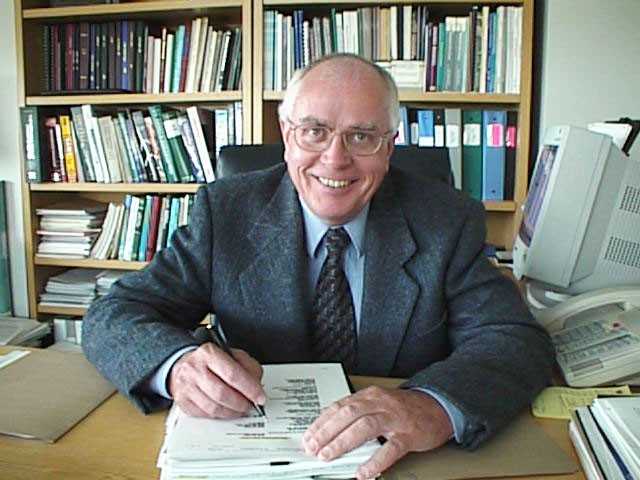
Few people have shaped the course of health research in Ottawa and beyond as profoundly as Dr. Ronald G. Worton. From discovering critical gene mutations to becoming the first CEO and Scientific Director of The Ottawa Hospital Research Institute (OHRI), Dr. Worton helped establish a culture of scientific excellence that continues to define our hospital today. When he arrived in Ottawa in 1996 to help build the hospital’s research program, he brought a collaborative vision that helped shape research at The Ottawa Hospital (TOH), and in the research community at large, for decades to come. And now, even in his retirement, Dr. Worton continues to give back and support the future of healthcare.
A trailblazer in genetic research
Dr. Worton’s path to medicine and research was anything but linear. Growing up in Winnipeg, Dr. Worton initially pursued physics. A chance carpool with biology students, who were energized by emerging discoveries about DNA, sparked his interest in biomedical research. That set him on a new path, first to a master’s degree in radiation physics at the University of Manitoba, and then to stem cell research for a PhD in Medical Biophysics at the University of Toronto.

Recruited to the newly established Genetics Department at Toronto’s Hospital for Sick Children, Dr. Worton emerged as a trailblazer in genetic research. As head of a research team, he helped discover the dystrophin gene, demonstrating that mutations in this gene cause Duchenne muscular dystrophy. At the time, gene discovery was still in its earliest stages, and this breakthrough helped lay the foundation for the Human Genome Project, a global effort to map all human genes and transform how scientists understand disease.
“What makes research thrive isn’t competition. It’s collaboration, shared ideas, and a willingness to support one another.”
— Dr. Ronald G. Worton
For Dr. Worton, what has been most meaningful is seeing how research into Duchenne muscular dystrophy has continued to advance over time, especially by scientists he recruited to OHRI. He notes the work of Dr. Michael Rudnicki, a senior scientist in regenerative medicine, and Director of the Sprott Centre for Stem Cell Research. Dr. Rudnicki’s team is conducting promising research that could one day lead to new treatment options with the potential to change the lives of children with muscular dystrophy.
When reflecting on this, Dr. Worton shares, “What makes research thrive isn’t competition. It’s collaboration, shared ideas, and a willingness to support one another.”
Contributing in new ways
This spirit of collaboration shaped Dr. Worton’s approach to leadership and to giving back. When he retired in 2007, colleagues, friends, and supporters came together to establish the Dr. Ronald G. Worton Researcher in Training Award. While it originally recognized outstanding research by students and postdoctoral fellows across all disciplines, the award is now focused on those trainees who specialize in lab-based research.
When considering how best to give back in support of our hospital, Dr. Worton noted that this Researcher in Training Award was supported by a strong endowment fund that was fulfilling its purpose, so he shifted focus to supporting our Campaign to Create Tomorrow. He saw the campaign as an opportunity to contribute to the future of healthcare in a meaningful way.
Now, with a $50,000 commitment, Dr. Worton has stepped forward, not only as a major donor, but also as a Campaign Patron. He hopes his gift will encourage other community leaders to follow suit, just as he was inspired by Campaign Patron and former long-time President and CEO of The Ottawa Hospital, Dr. Jack Kitts.
“Becoming a Campaign Patron felt like the right way to contribute and to support this next chapter. I hope that by stepping forward, I can inspire other leaders to give as well,” says Dr. Worton.
Passing the torch to young researchers
To this day, Dr. Worton remains deeply engaged with the hospital and research community he helped build. His support reflects a belief in what the new hospital campus and its research will make possible for patients, researchers, and our community for generations to come.
“In one way or another, I hope this gift supports young researchers, providing them with the space, tools, and opportunities they need to fuel the next generation of discovery.”
— Dr. Ronald G. Worton
That belief in the power of research has guided his distinguished career and is reflected in the honours he has received, including induction into the Canadian Medical Hall of Fame and appointment as an officer of the Order of Canada.
“In one way or another, I hope this gift supports young researchers, providing them with the space, tools, and opportunities they need to fuel the next generation of discovery,” says Dr. Worton.
Through his leadership and philanthropy, Dr. Worton is passing the torch — investing in discovery, empowering the next generation of researchers, and ensuring a strong future for healthcare in our community and beyond.






