Philanthropy runs deep in Joan Johnston’s family. In fact, it runs one hundred years deep. Her great-grandfather, Senator Lawrence Wilson, donated part of his property in 1923 to help create a park in the town of Coteau-du-Lac and built libraries and community centres in the region. Her mother, Josette Robertson, lived to 101 and inspired Joan through her lifelong commitment to giving back, particularly in support of healthcare. Today, Joan carries this legacy forward, guided by her own passions: protecting the environment and advancing medical research.
“If ever there were a cause that could benefit all of the residents of Ottawa and beyond, it is the new Ottawa Hospital.”
— Joan Johnston
“The Josette Robertson and Joan Johnston Family Foundation is pleased to contribute $3 million to The Ottawa Hospital’s Campaign to Create Tomorrow,” she says. “If ever there were a cause that could benefit all of the residents of Ottawa and beyond, it is the new Ottawa Hospital.”
It is critical to The Ottawa hospital to create a site that promotes health and healing – for the individual and for the environment. This transformational gift will support the hospital’s design plans for therapeutic gardens and green spaces and a Tiny Forest, alive with birds and butterflies — aspects of the project that are of particular importance to Joan.
“These plantings, the Tiny Forest and green spaces are a contribution not only to the hospital community of patients, staff, and visitors, but also to the environment and community for generations to come,” says Joan.
Joan’s commitment to Tiny Forests spans the city. Through partnerships with Forêt Capitale Forest and EnviroCentre, her foundation has transformed schoolyards and community housing sites into thriving ecosystems that grow rapidly, enrich the soil, and foster biodiversity.
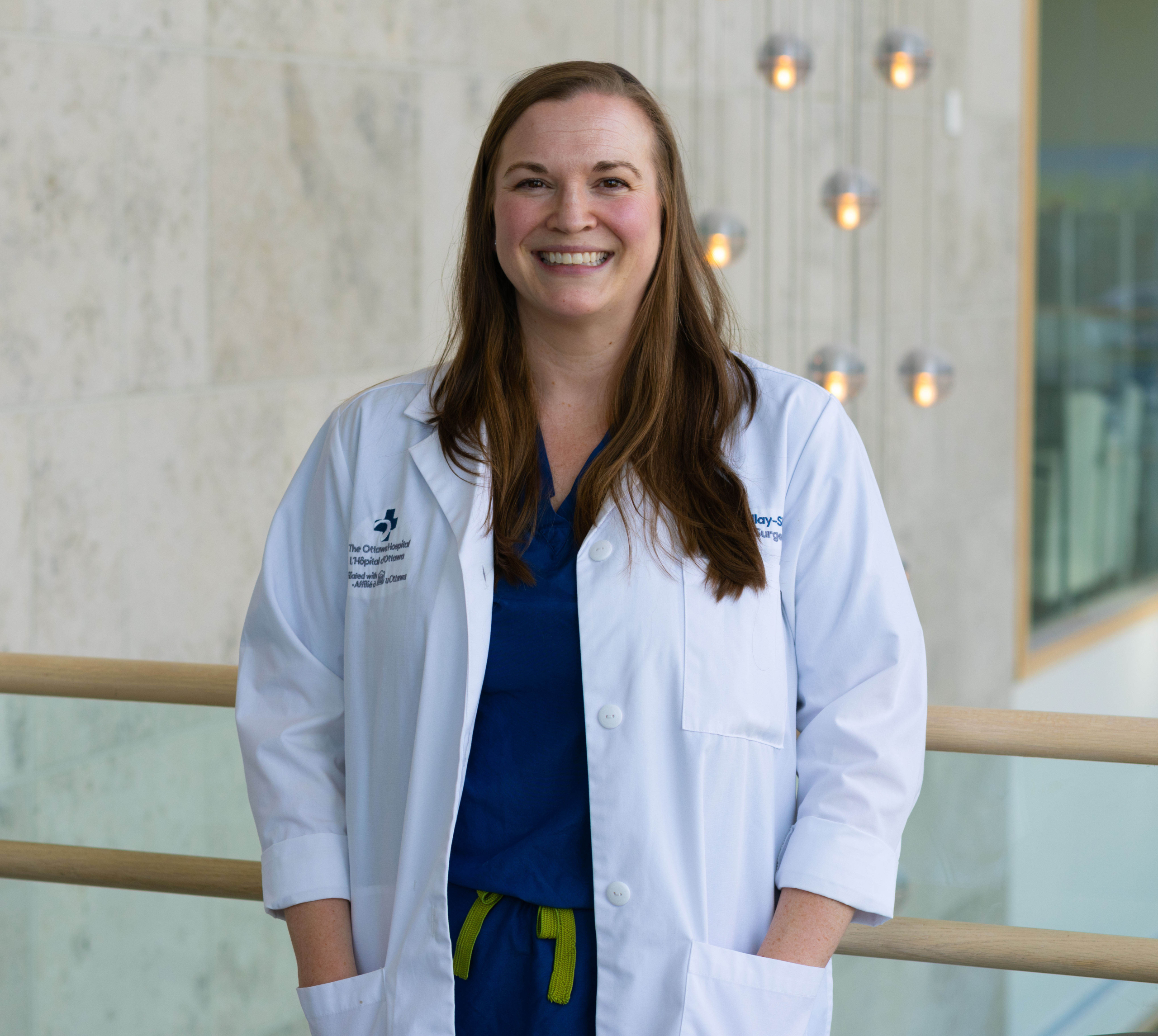
While this gift focuses on the environment, it also aligns with Joan’s longstanding support for regenerative medicine. After her cousin’s son suffered a severe accident at 19, she became a champion of Dr. Eve Tsai, a neurosurgeon at The Ottawa Hospital, and her spinal cord injury research.
“I couldn’t do anything specifically for him,” Joan says, “but I went looking for someone I could support who was doing research in that area. Dr. Tsai is brilliant and compassionate — and I was very happy to provide support for her work.”
For Joan, caring for the environment and supporting medical research come from the same place: a belief in healing and hope.
“It doesn’t matter to me if my name is attached to it,” she says. “What matters is that we create an environment that is sustainable and beautiful and will benefit citizens of the city for years to come. That is my gift to the city.”
With this extraordinary gift, Joan Johnston is helping to create a hospital that is more than a place of treatment — it will be a sanctuary where nature and care come together to restore body, mind, and spirit. And when the time comes to break ground, Joan plans to be there, shovel and all.
“Oh, I’ll be there on my hands and knees with a trowel,” she says. “I wouldn’t miss it.”