Published: February 2025
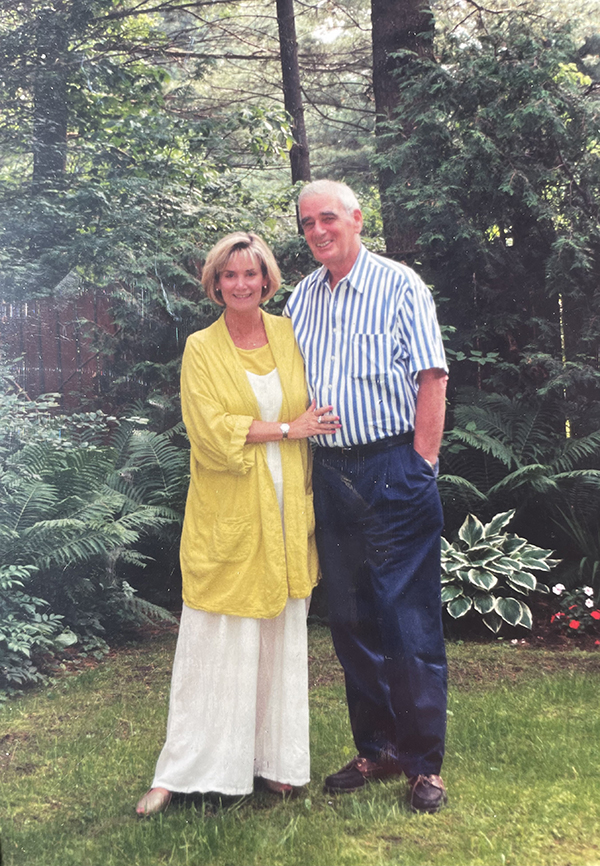
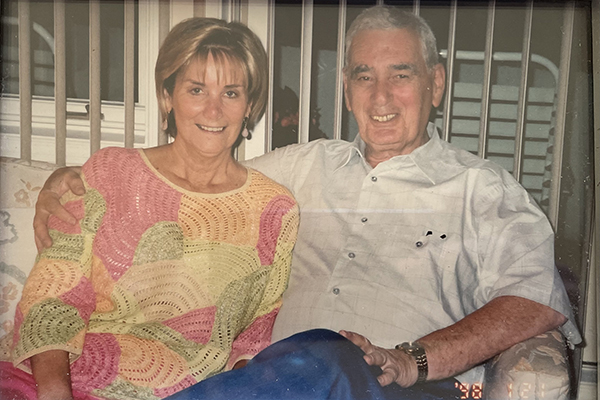
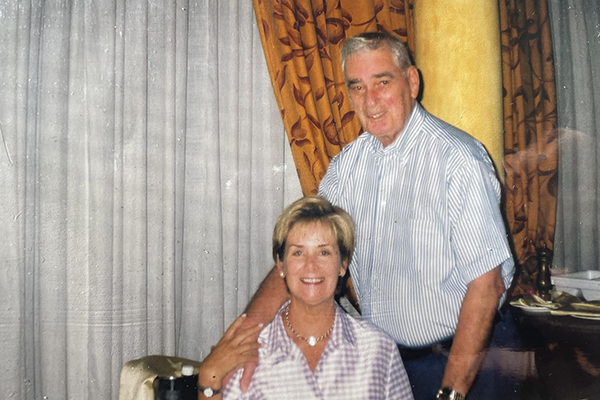
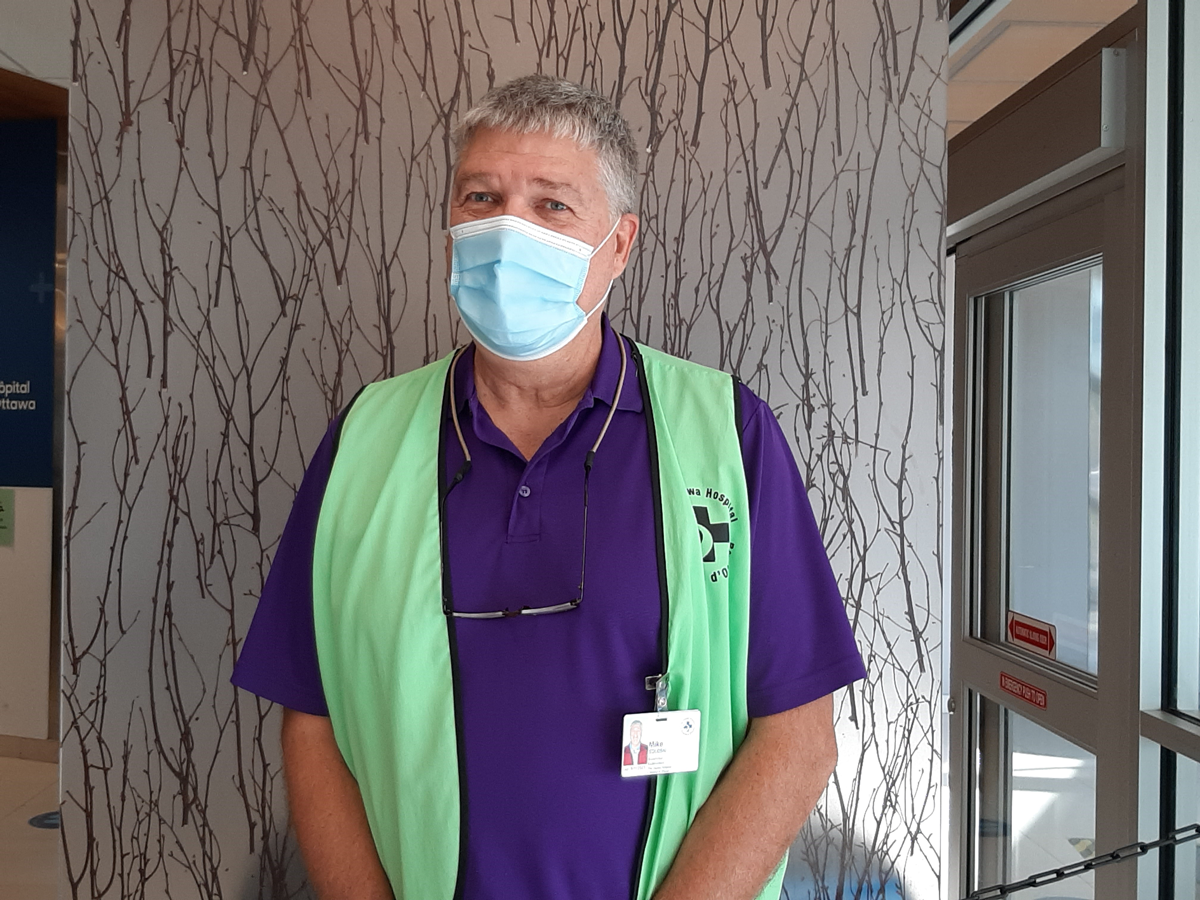
When Joanne Workman makes the short walk to the Civic Campus of The Ottawa Hospital for her volunteer shift, she gets a firsthand look at the construction progress of the future site of our new hospital campus. Through her dedicated weekly volunteering and her financial support, Joanne is helping to create a better tomorrow for generations to come.
Healthcare is something that has always been close to Joanne’s heart. Growing up in Merrickville, she’d watch her mom, Helen McKenna, dedicate herself to caring for patients at the former St. Francis Hospital in Smiths Falls. Helen was a devoted mother to seven children and a committed nurse who loved her job.
It was a career that started when she was very young and under challenging circumstances. Joanne recalls her mom telling her and her siblings stories about her time served during World War 2, caring for injured soldiers during the blitz. “Mom said she was never scared. ‘When you’re young, you’re not scared,’ she’d say,” recalls Joanne.
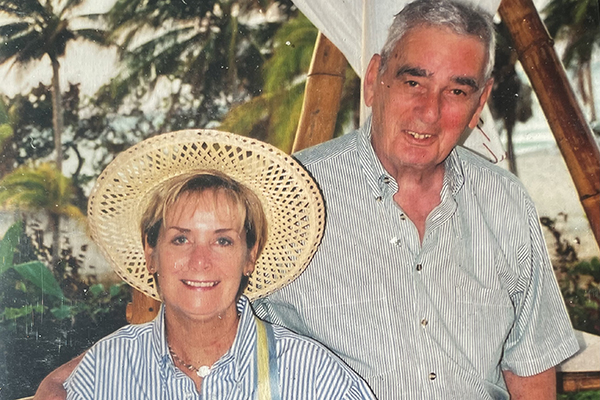
There was a time when Joanne considered a career as a nurse, but ultimately, she went in the direction of teaching and then accounting. She travelled across Canada with her work and then throughout the world with her husband, who was working in Yemen and Indonesia for the World Bank.
Giving back through volunteering
Giving back also came naturally to Joanne, and she even spent over a year volunteering with CUSO in Jamaica. When she settled back in Ottawa, not far from the Civic Campus, she decided to inquire about wearing the blue vest — attire that clearly identifies our dedicated volunteers around each hospital campus.
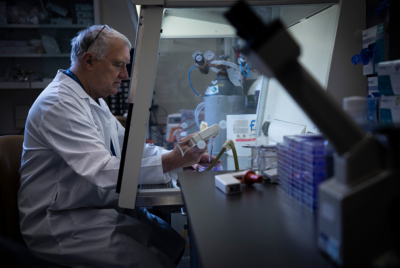
"Because I see the need firsthand — the need is so great. And we must support research and innovation at the hospital. This is not a little hospital; this is a major hospital research centre.”
— Joanne Workman
Volunteers are a vital part of our hospital. There are approximately 800 volunteers who help at our information desks, recreational therapy, inpatient and outpatient units, office helpers, as well as pet therapy. Volunteering is something Joanne tends to gravitate towards.
“I love to volunteer — I always have over the years. Every Monday you’ll find me here at the information desk, sometimes a little more in the summer months when the curling season is over,” explains the avid curler.

Now in her eighth year of volunteering, this isn’t the only way Joanne gives back to our hospital, she’s also a monthly donor. “I started doing that a couple of years ago because I see the need firsthand — the need is so great. And we must support research and innovation at the hospital. This is not a little hospital; this is a major hospital research centre,” says Joanne.
Monthly giving leads to a gift in will
Monthly support to our hospital is vital. This steady source of income fuels research discoveries and allows us to ensure patients have access to the most cutting-edge equipment and technology available. “It’s one of the best things I could do. And I just feel really good about it,” says Joanne.
When the time came for Joanne to rewrite her will, she spoke with her financial advisor, and learned more about the impact of a leaving a gift in her will to charity and the benefits to her estate. By donating to a charity, it reduces the taxes paid by your estate.
“When I see what happens every day as I’m volunteering, and see the care that’s happening, it inspired me to leave a portion of my estate to the hospital.”
— Joanne Workman
Gifts in wills serve two purposes:
- First, remembering The Ottawa Hospital in your will is a wonderful way to reshape the future of healthcare by providing much-needed funding.
- Second, it stretches your lifetime of generosity into the future. We often hear from donors that they feel deeply satisfied, knowing they can continue to help their families and neighbours even after they’re gone.
For Joanne, leaving a gift to The Ottawa Hospital made sense to her. “When I see what happens every day as I’m volunteering, and see the care that’s happening, it inspired me to leave a portion of my estate to the hospital.”
New hospital campus inspires legacy gift
Her decision is also about the excitement of what’s still to come and what the Campaign to Create Tomorrow will mean — funding the new hospital campus and taking leading-edge research to the very top tier in the world.
Watching the progress at the construction site inspires Joanne. “We need a new hospital. It’s amazing how it’s growing out of the ground. I’m told that directions should be easier for the new hospital because of the way they’re laying it out, it’s going to be much easier for people to get around. Right now, you’re dealing with buildings that have all just been patched together over time, in order to expand.”
“We, as a community, don't realize how many people come and go through the hospital. Patients get cared for and sent home, and they're happy. But the hospital needs money to do this and to continue to expand, especially for the research.”
— Joanne Workman
The Ottawa Hospital’s new campus is Ottawa’s largest-ever healthcare infrastructure project and will be built on a 50-acre site bordered by Carling Avenue, Preston Street, and Prince of Wales Drive, near Dow’s Lake in Ottawa. While it’s already one of the best hospitals in Canada, The Ottawa Hospital is striving to earn it’s place in the very top tier of global healthcare leaders.
“We, as a community, don’t realize how many people come and go through the hospital. Patients get cared for and sent home, and they’re happy. But the hospital needs money to do this and to continue to expand, especially for the research,” says Joanne. “I am blown away with all these diagnostics they do there, and that makes a huge difference. But all these things don’t just happen.”
Building a new hospital is a once-in-a-generation opportunity. Along with a new outpatient care and research building, this modern, accessible, and technologically advanced healthcare facility is being built for our community, by our community.
Joanne is eager to step into the new hospital campus as a volunteer, and seeing how it all comes together. It’s for forward-thinking people like her, who will create a legacy for generations to come.