SEPTEMBER 1, 2020 OTTAWA, ON – If you thought The Ottawa Hospital might postpone its annual President’s Breakfast in light of COVID-19, you’re in for a wake-up call. That’s because today, The Ottawa Hospital Foundation announced its influential fundraiser is once again blazing a new trail. For the first time since its inception in 2001, the annual one-hour event will be held virtually on Tuesday, September 29, from 8 a.m. to 9 a.m. in a groundbreaking online adaptation of the traditional in-person gathering.
HIGHLIGHTS:
- This year’s event will be held virtually on Tuesday, September 29, from 8 a.m. to 9 a.m.
- Since 2001, The Ottawa Hospital’s annual President’s Breakfast has raised nearly $12 million toward leading-edge research, facilities, equipment, and tools to improve patient care.
- The President’s Breakfast is a one-hour coming-together of guest speakers, front-line healthcare researchers, patients whose lives have been saved, and more than 500 dedicated supporters to raise critical funds for The Ottawa Hospital.
While COVID-19 has put events of this nature on hold, the need to raise crucial funds for research and patient care not only continues, it is amplified by the pandemic.
As has become tradition, the President’s Breakfast will spotlight some of the year’s most incredible, inspiring stories of hope and compassion to an audience of more than 500 dedicated supporters – including lead sponsor Doherty and Associates.
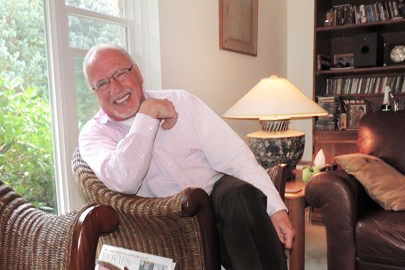
“We may not be able to physically be together in the same room, but we can still gather as a community and connect via live streaming video for this great cause,” said Tim Kluke, President and CEO of The Ottawa Hospital Foundation. “Make no mistake, this will not look or sound anything like your run-of-the-mill video conference call. We’re employing state-of-the-art technology to make it the next best thing to an in-person event. It is an extremely important component of our yearly fundraising calendar, and so we have worked hard to create a dynamic program of guest speakers, special announcements, and a few surprises to make sure we stay true to the innovative spirit for which the President’s Breakfast is well known.”
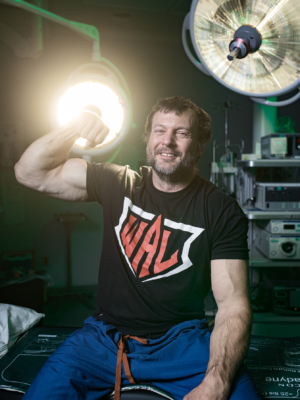
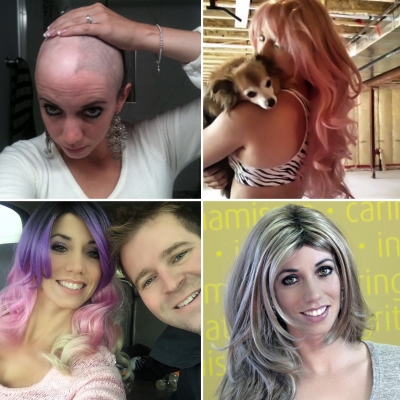
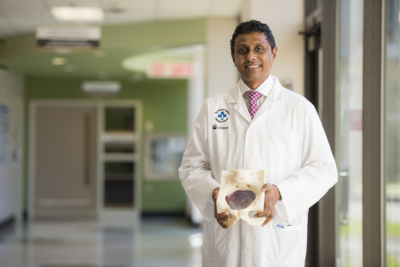
The President’s Breakfast will also mark the first official address from Cameron Love, the new President and CEO of The Ottawa Hospital, as part of its itinerary of guest speakers and former patients including Stuntman Stu, who recently underwent his second bone marrow transplant at The Ottawa Hospital in his battle with leukemia.
With a rich history, this event has raised close to $12 million over the past 18 years in support of healthcare in Ottawa. In 2018 alone, more than $800,000 was donated in just one inspiring morning. Viewers can donate online in a variety of ways: with a monthly gift, a multi-year commitment, or a one-time tribute donation in support of The Ottawa Hospital.
The President’s Breakfast in support of The Ottawa Hospital will happen Tuesday, September 29, from 8 a.m. to 9 a.m.
About The Ottawa Hospital:
The Ottawa Hospital is one of Canada’s top learning and research hospitals, where excellent care is inspired by research and driven by compassion. As the third-largest employer in Ottawa, our support staff, researchers, nurses, physicians, and volunteers never stop seeking solutions to the most complex healthcare challenges.
Our multi-campus hospital, affiliated with the University of Ottawa, attracts some of the most influential scientific minds from around the world. Our focus on learning and research leads to new techniques and discoveries that are adopted globally to improve patient care.
We are the Regional Trauma Centre for eastern Ontario and have been accredited with Exemplary Standing for healthcare delivery — the highest rating from Accreditation Canada. We are also home to world-leading research programs focused on cancer therapeutics, neuroscience, regenerative medicine, chronic disease, and practice-changing research.
Backed by generous support from the community, we are committed to providing the world-class, compassionate care we would want for our loved ones.
For more information about The Ottawa Hospital, visit ohfoundation.ca.