Published: March 2025
Imagine the sensation of a sudden, sharp electric shock to your face, intense and unyielding. Now, imagine that happening repeatedly, day after day, without any warning — pain so excruciating it brings you to your knees. This was a daily struggle for Michelle Kupé. After months of testing, she was diagnosed with trigeminal neuralgia, a rare condition that had a debilitating effect on her life. Desperate for relief, she sought help from The Ottawa Hospital’s neurosurgery team, hoping to regain control of her life.
In December 2017, Michelle scheduled an appointment with her dentist to investigate a strange buzzing sensation in her cheek, which she initially thought was a tooth infection or dental problem. After taking x-rays, the dentist found no issues with her teeth, but the sensation persisted, leaving Michelle with the feeling that something wasn’t right.
By the time the new year arrived, Michelle was preparing to set off on a cruise with her girlfriends. However, the persistent buzzing sensation and the overall sense that something wasn’t right led her to return to the dentist’s office. With no clear explanation for the strange sensations, she was prescribed antibiotics to rule out a sinus infection or other potential issues. During her trip, Michelle couldn’t shake a nagging thought. “The entire time I was there, I kept thinking, ‘Something has happened to me… and I’m not well.’ I was deeply aware that my life was taking a different turn. Something was wrong.”

Trigeminal neuralgia’s excruciating progression
As the buzzing sensation and pain intensified, Michelle returned to the dentist for a third time. It was then the dentist suspected the symptoms might suggest a rare condition called trigeminal neuralgia — a condition that causes severe, electric-shock-like pain on one side of the face. The dentist advised her to make an appointment with her family doctor and see a neurologist as soon as possible.
“It went from this buzzing sensation in my face to feeling like I was being electrocuted. It felt like I was being stabbed, like an electric current was running through my face.”
— Michelle Kupé
As she waited to see a neurologist, the symptoms worsened. “It went from this buzzing sensation in my face to feeling like I was being electrocuted. It felt like I was being stabbed, like an electric current was running through my face.”
As each attack eased, Michelle was terrified to touch or move any muscle in her face, fearing the pain would return. Eventually, she saw a neurologist, who confirmed that she had trigeminal neuralgia. But while one mystery was solved, another emerged. There are three potential causes for this condition: multiple sclerosis, a brain tumor, or vascular compression.
All about trigeminal neuralgia
As Michelle waited for an MRI, she continued to run her successful real estate business and care for her five children. Her condition remained stable with medication into the spring of 2018, with occasional, painful flare-ups. But, as time progressed, things started to deteriorate quickly, with attacks becoming more frequent and debilitating. Eating, brushing teeth, and even smiling were becoming unbearable.
“I remember thinking, I don’t think I’m going to be able to go on. Something as simple as a light breeze could cause an attack,” she recalls. “With thoughts of another winter approaching, my husband and I talked about moving somewhere warm because I couldn’t imagine a cold wind hitting my face.”
Debilitating shocks to Michelle’s body
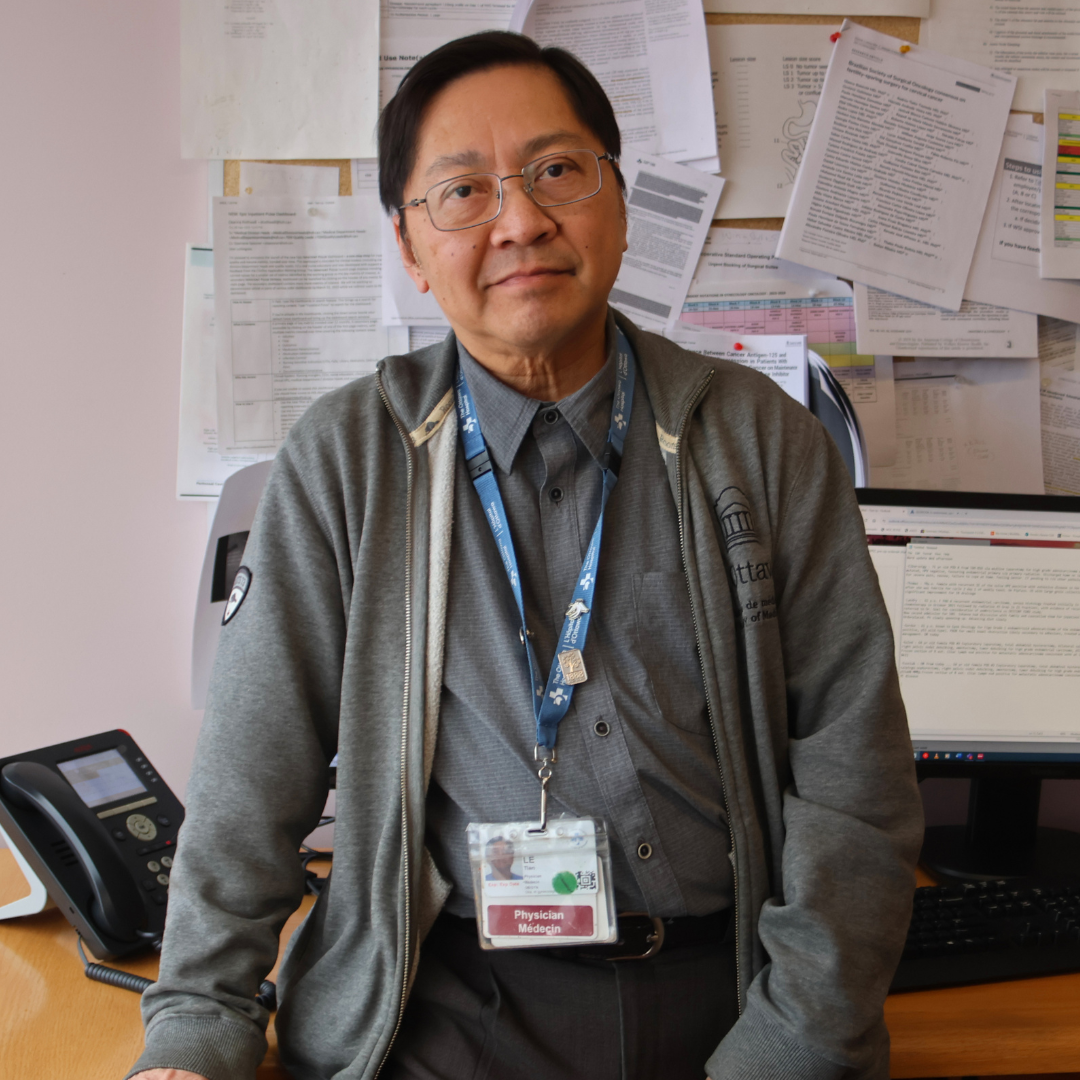
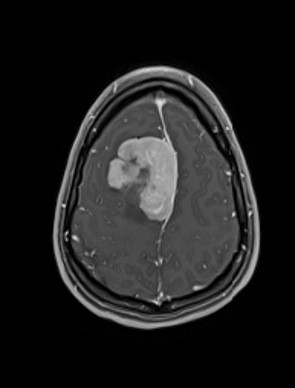
MRI results eventually revealed her condition was the result of a vascular compression and she was referred to Dr. Adam Sachs, current Division Head of Neurosurgery at The Ottawa Hospital.
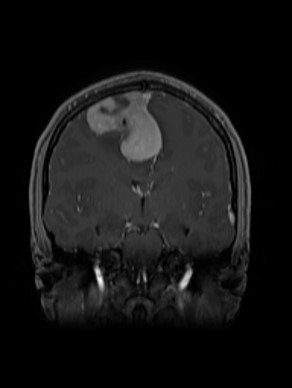
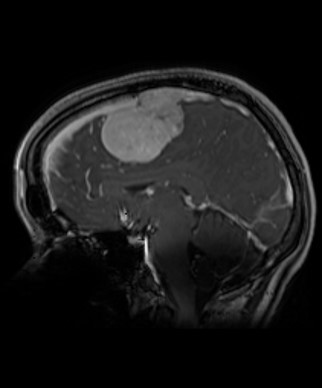
Dr. Sachs and his team see patients for a wide variety of facial pain, but he says trigeminal neuralgia can be one of the worst. It affects the trigeminal nerves, which carry signals from the face to the brain, and causes intense pain like an electric shock on one side of the face. “The MRI showed that a vessel loop of an artery that goes to the brain stem and cerebellum was compressing the trigeminal nerve — that was the cause of the pain,” he explains.
Director of Neuromodulation and Functional Neurosurgery and Scientist at The Ottawa Hospital
“It feels like a high voltage electrical shock running through your face or some people describe it as a dagger being jammed into their face.”
— Dr. Adam Sachs
For patients, like Michelle, the condition can be unbearable. “It feels like a high voltage electrical shock running through your face, or some people describe it as a dagger being jammed into their face,” explains Dr. Sachs. “People are using those terms not to be colourful, but because that’s the closest thing they can come up with, and we hear these terms again and again.”
Modern microsurgical technique with the help of Teflon
While surgical treatment has been available for decades, recent advances have provided new treatment options — modern microsurgical techniques that are more effective and safer. As Dr. Sachs explains, the tools they have today are state-of-the-art.
When it comes time for surgery, it’s an intricate procedure with the patient’s head turned because the surgical team must access a small space at the back of the head called the cerebellopontine angle or CP angle. “That’s where we see all the nerves and the arteries that go to very critical structures of the brain stem. It’s close to the facial nerve, and if damaged, it results in facial palsy.”
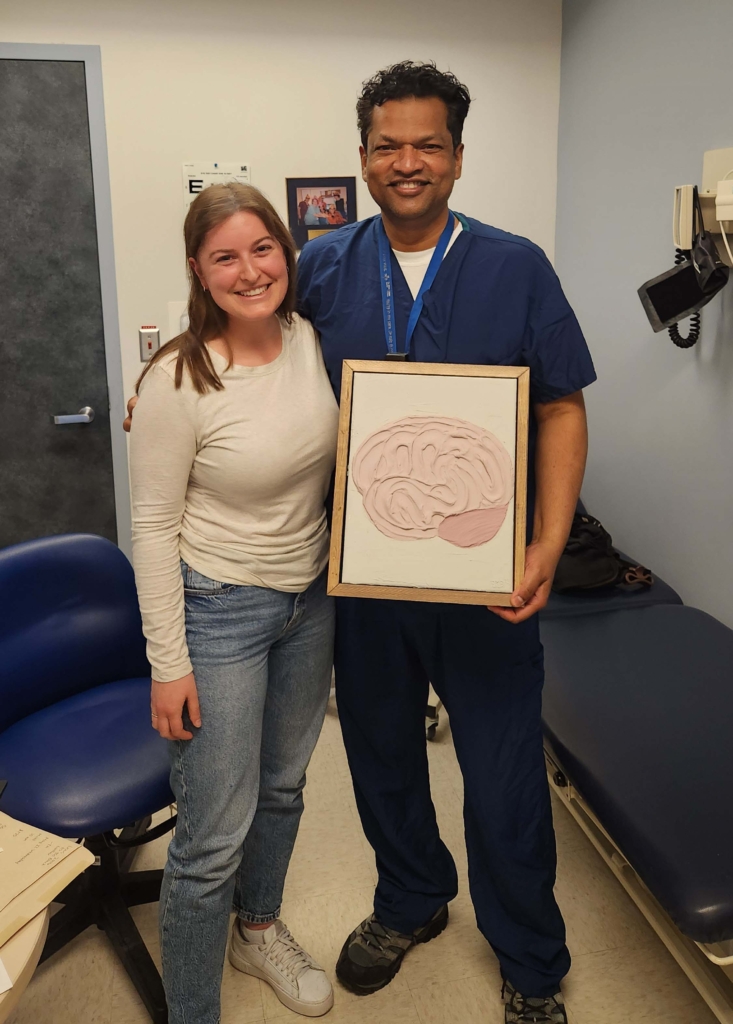
In Michelle’s case, the artery had a large vein wrapped around the nerve, and so Dr. Sachs called in his colleague Dr. John Sinclair to assist with the surgery because of the complexity.
“We decided even though it was a large vein, to carefully dissect it off the nerve in addition to the artery. Then we put little Teflon pads under both the vein and the artery to keep them away from the trigeminal nerve,” says Dr. Sachs.
The Teflon creates a physical barrier that will keep the vein and the artery from the nerve, but also keep the blood flowing through them, so they will continue to function.
“We tear it up to microscopic pieces of the Teflon, shaped like cigars, and it creates a barrier because it stays — it’s not going to absorb into the body,” explains Dr. Sachs.
For the most complex parts of the procedure, the neurosurgical team uses high-magnification microscopes and microscopic knives.
Pain is an invisible disease
When it comes to cases of trigeminal neuralgia, our hospital sees patients from across Eastern Ontario. According to Dr. Sachs, not all cases are debilitating like Michelle’s, but for many, the pain they are experiencing is made worse by the fact that those around them don’t always understand what the patient is going through.
"She wasn't even able to smile or laugh for a year. Every time she would smile, she’d have these attacks and pain. So, treating pain is rewarding as a physician because we're able to help relieve it, and that can be transformative for the patient.”
— Dr. Adam Sachs
“Michelle is a very personable individual. She loves to be around family, friends and to laugh and enjoy life. She wasn’t even able to smile or laugh for a year. Every time she would smile, she’d have these attacks and pain,” explains Dr. Sachs. “So, treating pain is rewarding as a physician because we’re able to help relieve it, and that can be transformative for the patient.”
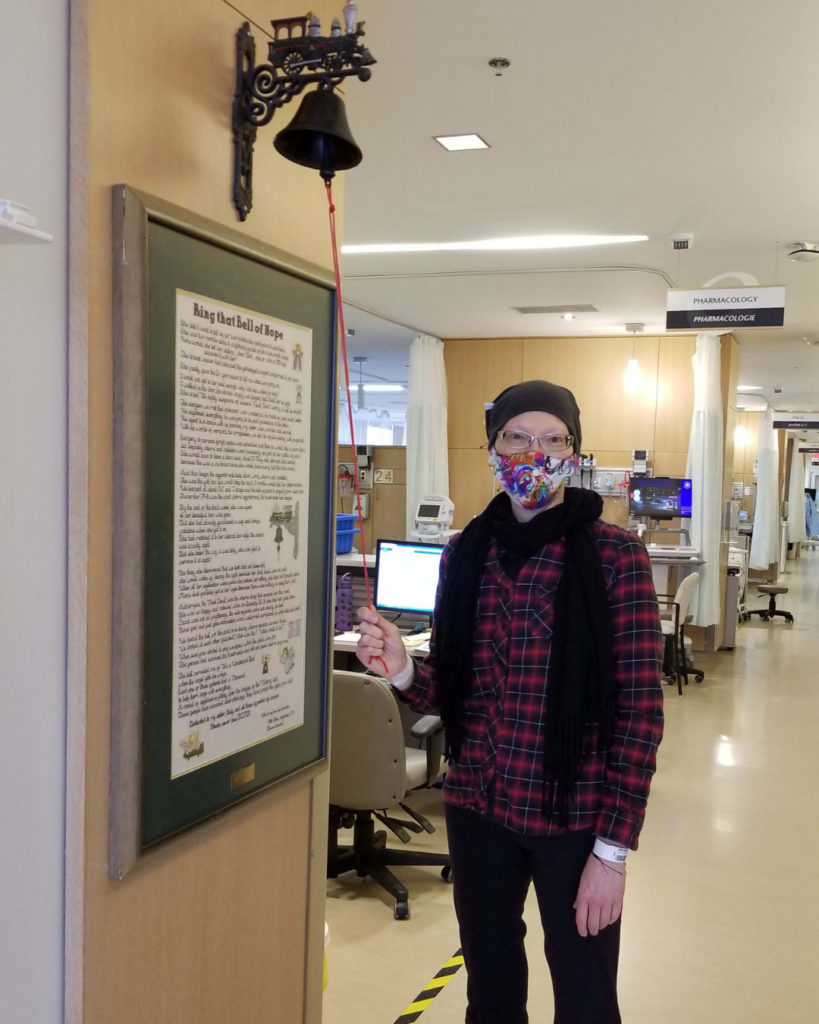
“I remember waking up from surgery and knowing immediately that I didn’t have electricity running through my face. The relief was immediate,” says Michelle.
"The relief was immediate."
— Michelle Kupé
The gratitude she feels runs deep, not only for those who helped take away the agonizing pain, but also for the nursing staff in the neuro ICU — she can’t remember all their names, but she will never forget their compassion.
“This one particular nurse was so kind. I remember slowly waking up after the surgery with him rubbing my arm and saying, ‘You’ve had a rough day today, but you did great,’” she says. “I felt encompassed by caring people who had my best interests at heart. I never for a moment felt abandoned when I was at my most vulnerable.”
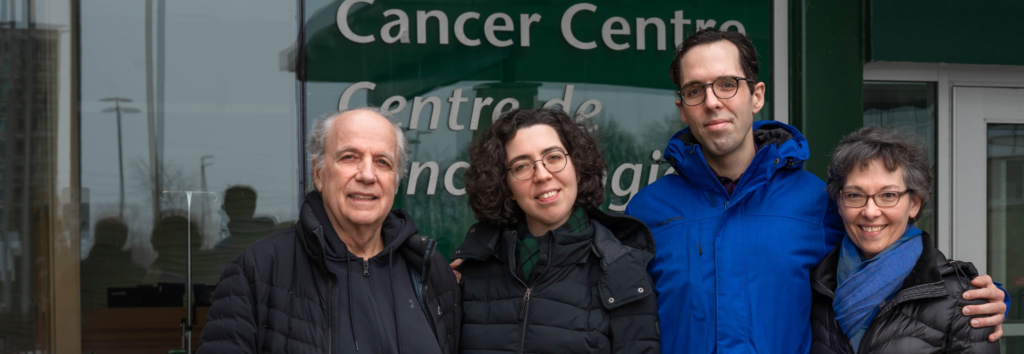
Regaining her life back
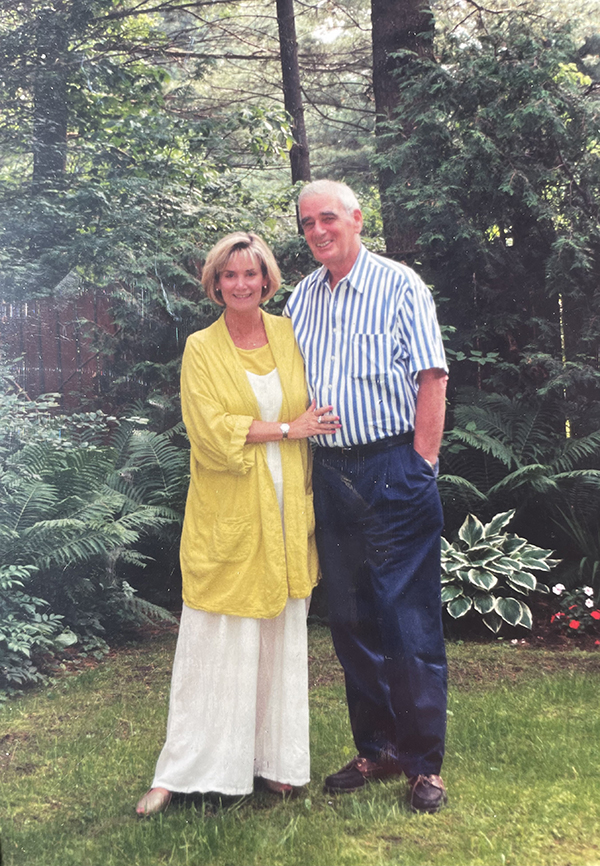
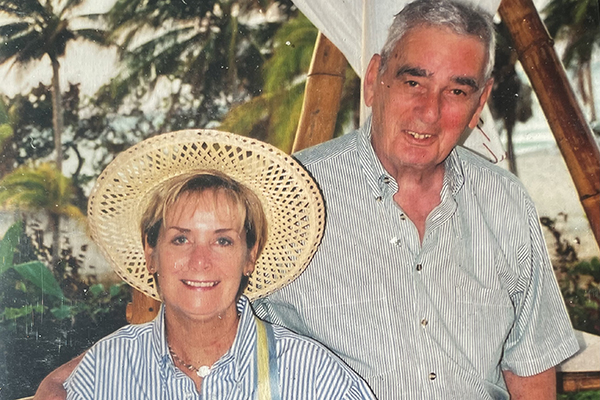
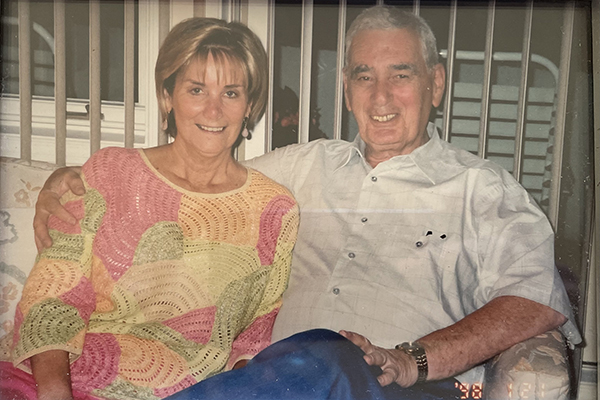
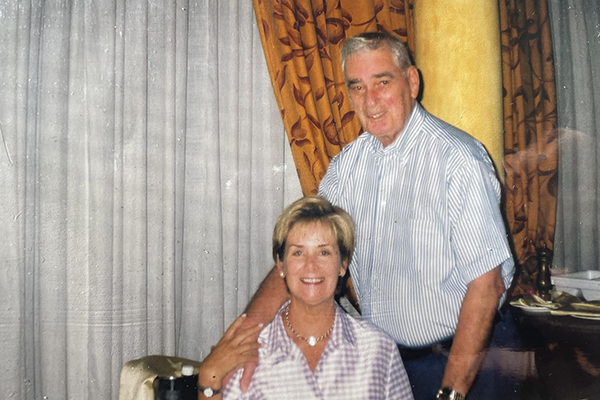
After five days in the hospital following her surgery, Michelle returned home to her five children and husband Rob. Within five months, she was able to return to work, but continued with physiotherapy for about a year. Today, she can experience bad headaches and is still seen by the pain clinic, but she’s living a full life again — now as an empty nester with her kids grown up and exploring the world.
Michelle reflects on a full circle moment from many years ago when her parents first heard about Dr. Sinclair returning from the United States to his hometown of Ottawa and his efforts to bring a CyberKnife radiosurgery robot to our hospital.
“My parents heard about this CyberKnife and they rallied to support his efforts. Who would have known that years later the neurology department would be where their daughter would end up? We had no other connection really with neurology at the time, and yet this emerging neurosurgery tool was something my parents were really passionate about making sure people had access to.”
It’s a perfect example of the impact of philanthropy and never knowing who it will benefit.
“We believe things don’t happen by accident. The way it lined up and how it all unfolded was part of the plan for my life and shows it’s important to keep giving back.”