Sadly, Kelda Whalen passed away on August 27, 2025. We are grateful for her generosity to our hospital and the legacy she leaves behind.
Published: August 2025
Read time: 3 mins
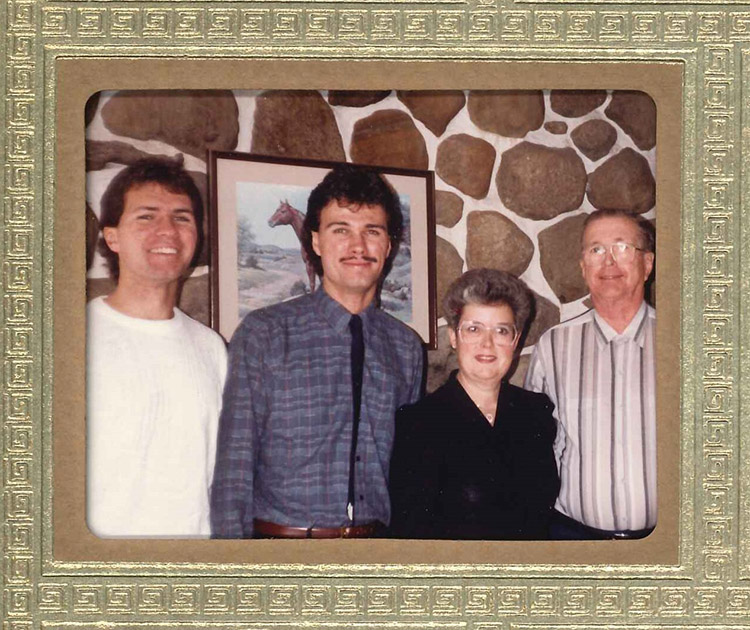
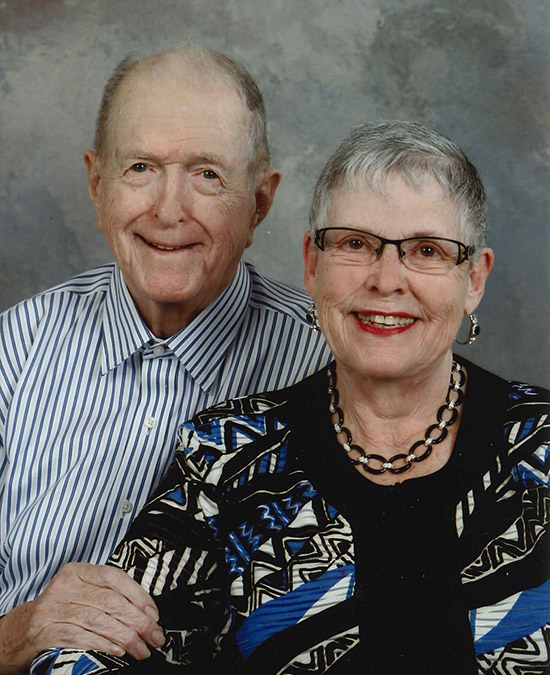
If Kelda Whalen were to place a dot on a map of the world for every location she has been, there would be an abundance of dots. Between her dedicated work in the foreign service and her love of travel, she has travelled the world extensively — but always returned to her hometown of Ottawa. That’s where she’s enjoyed the beautiful landscape, the arts community, and giving back to charities and organizations that were important to her, including The Ottawa Hospital.
Born in Ottawa at the Civic Campus, her travelling instincts came naturally, thanks to her father who was in the Canadian Armed Forces. Her family constantly moved across Canada to different military bases during her childhood years, and her father’s work even took them to Germany twice.
By the time she turned 21, she wrote the foreign service exam on a whim. She passed and that launched her career into quite a different direction than she thought when she was growing up. “Originally, my plan was to go to library school, but life had a different path for me,” says Kelda.

Exploring the world, but Ottawa was always home
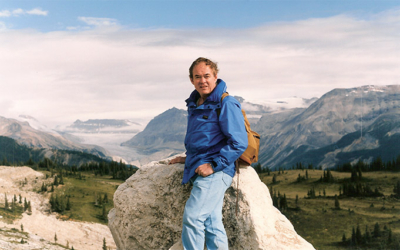
Over the next decade or so, she was posted around the world. Each city bringing a unique opportunity she’d never forget. Kelda’s first posting was Dublin, Ireland. “It was a delightful place, even though it rains all the time,” recalls Kelda.
Next stop was London, England — a city she thoroughly loved. “I was there at a fortunate time when the dollar was up, and the pound was down. This allowed me to explore my love of arts, and I got to enjoy all these fabulous plays.”

After four years in England, Kelda was stationed in New Delhi and then Hong Kong. Afterwards, she returned to Ottawa for a short time before one of her superiors made her aware of a temporary posting in Beirut. “I immediately said, ‘I want it!’ It was 20 above Celsius in Beirut that day and 20 below in Ottawa, so I took it.”
This deployment was a different experience than any other. Despite it being dangerous at that time because of political unrest, she was still able to tour the surrounding countryside, which she recalls as being quite lovely.
A devastating turn of events
Her last big trip was to Damascus, and then she returned to Ottawa in between deployments. It was the summer of 1982, and while there were plans for her to be deployed once again, life took a dramatic turn on one hot summer evening.
After a Saturday evening swim at the pool in her apartment building, she decided to go into the sauna. “I had only taken two saunas in my entire life, and why I decided to go into the sauna, I don’t know. I had low blood pressure — I was overcome by the heat, and I fainted,’ recalls Kelda.
She got up right away but subsequently fainted four more times before falling against the door of the sauna and onto the locker room floor. “I managed to get myself up and thought it was odd, but overall, I didn’t feel unwell. It turns out by fainting five times in a row, I damaged a part of my brain called the basil ganglia, which controls the body’s ability to move.”
Diagnosed with dystonia after fainting multiple times
Within two days, despite feeling fine, Kelda looked in the mirror and she could see the muscles in her neck standing out as though they were spasming.
Sadly, it took many years, before she learned what had happened. Finally, in 1996, she was diagnosed with dystonia. It is an uncommon neurological condition that causes muscles to contract uncontrollably, leading to twisting movements, abnormal postures, or repetitive motions. These muscle contractions happen because the brain sends faulty signals to the muscles, even when the person doesn’t intend to move.
At the time, Kelda was referred to a Toronto hospital and to Dr. Andres Lozano, well-known globally for deep-brain stimulation surgery. Unlike today, it was a time when Ottawa didn’t have the capacity or expertise for this.
“I was 31 when I first fell. That ended my career in the foreign service — I couldn’t go abroad because I was in pain from the spasms. I’ve had multiple neurosurgeries over the years at The Ottawa Hospital, but sadly, none have been able to alleviate the symptoms of dystonia.”
But this condition didn’t stop Kelda completely. She persevered and continued to work part time as an immigration officer before she retired in 2002.
She also didn’t let dystonia hold her back from travelling, which she continued to do extensively with friends. As travelling became more difficult, she shifted to cruises and then van excursions. She’s visited Venice, Italy three times — it’s her all-time favourite destination.
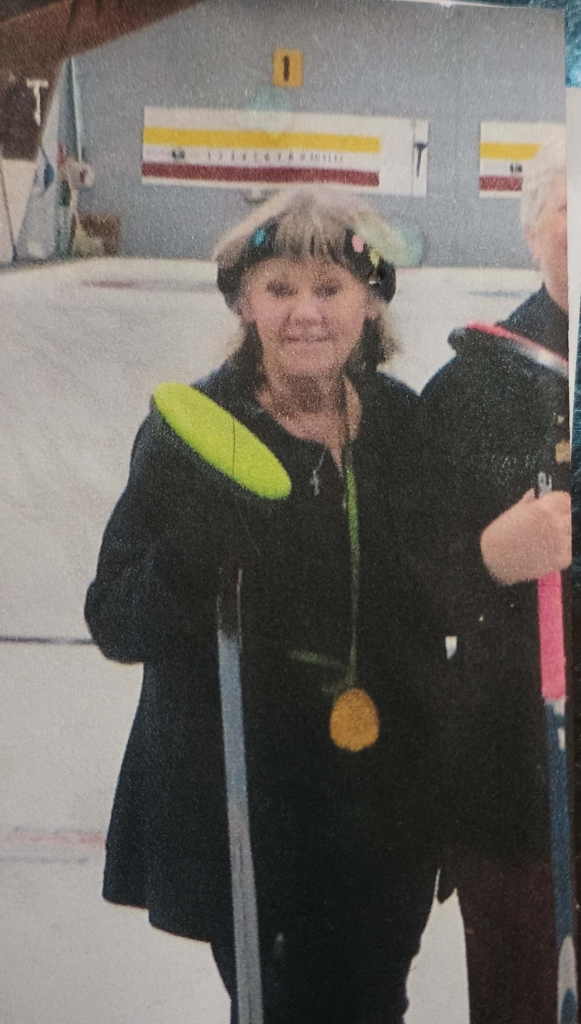
“As I get older, I have more and more difficulty walking. I had an A-linker, known as a walking bike, from 2019 to 2023, and I’d go out every morning at 6 a.m. because I’m an early riser. I liked to go out along the canal and enjoy the early morning peace.”

Finding a way to be remembered when she’s gone
But even her morning excursions have become more challenging over time as her ability to walk deteriorated and falls were more frequent. Despite the increasing difficulty, it didn’t stop her from getting out. In fact, it was during one of her walks that she began to think about her legacy and how she wanted to be remembered when she was gone.
“When I spoke to my financial advisor, she talked to me about the new hospital and the opportunity to have a patient room named after me, and that’s when I decided to leave a gift in my will to the Campaign to Create Tomorrow.”
— Kelda Whalen
“I wanted to leave a sign, and it was during a walk to the Governor General’s front garden when I saw benches with small plaques to say they’ve been donated by someone,” says Kelda. “When I spoke to my financial advisor, she talked to me about the new hospital and the opportunity to have a patient room named after me, and that’s when I decided to leave a gift in my will to the Campaign to Create Tomorrow.”
As a longtime patient of The Ottawa Hospital, including for multiple neurological surgeries over the years, the idea of single-patient rooms for the new hospital campus is certainly appealing to Kelda.
"I just want people to remember me when I’m gone.”
– Kelda Whalen
As someone who has always donated to organizations in her community, including the arts, supporting others with dystonia, as well as our hospital, by leaving a gift in her will, Kelda will always be remembered for reshaping the future of healthcare. Her name will be seen by other patients, their families, staff, and physicians who walk by the room that will be named after her when the new hospital campus opens. It’s a fitting way to help future patients who will need the hospital like she has.
Despite her health continuing to deteriorate, she continues to think of others. “Maybe I’ll get a patient room in neurology named after me, but I’m not too fussy, where it will be. I just want people to remember me when I’m gone.”