Published: October 2025
Read time: 3 mins
Published: October 2025
Read time: 3 mins
When Danika Fleury decided to move to Ottawa to kick off her teaching career, it was about having the opportunity to experience a big city. Little did she know, at such an early stage in life, she would need access to a hospital that specializes in complex medical care. From an early-stage breast cancer diagnosis to endometriosis surgery, The Ottawa Hospital was ready when Danika needed answers.
This elementary school teacher at Broadview Public School grew up in Sudbury, Ontario, and made the move to Ottawa in 2014. Since then, she has loved living in Canada’s capital — exploring the green spaces, bike paths, and all the festivals our city has to offer.
At the end of summer in 2021, Danika and her fiancé were planning to elope to British Columbia. Leading up to that time she noticed a lump in her breast seemed to be getting bigger. “I’ve always had lumps in my breasts. So, from time to time I would have an ultrasound, and there was never anything to worry about. But this one lump was bigger than the rest, and seemed to be growing,” explains Danika.
Discovery of a growing lump

Her doctor suggested an ultrasound and she and her fiancé went ahead with their wedding plans and enjoyed a beautiful ceremony. “It was enchanting — like a fairy tale. During that amazing trip, I do remember thinking ‘What if I have cancer?’ Then I thought, ‘I’m young and I’m healthy. This doesn’t happen to young people.’”
Upon her return, and back to the classroom, it was well into the fall when she finally booked the ultrasound. Within hours of that test, Danika received a call about scheduling a biopsy. “Immediately my heart sank.”
“I had been worried, but I really didn’t think it was going to happen. I was only 30 years old. That’s when everything changed.”
— Danika Fleury
By the new year, Danika received the news she never expected to hear, she had breast cancer. It was on the day of her biopsy, our specialized team conducted an ultrasound and discovered a smaller hidden lump which turned out to be cancerous. The initial lump was benign. “I was shocked. I had been worried, but I really didn’t think it was going to happen. I was only 30 years old. That’s when everything changed.”
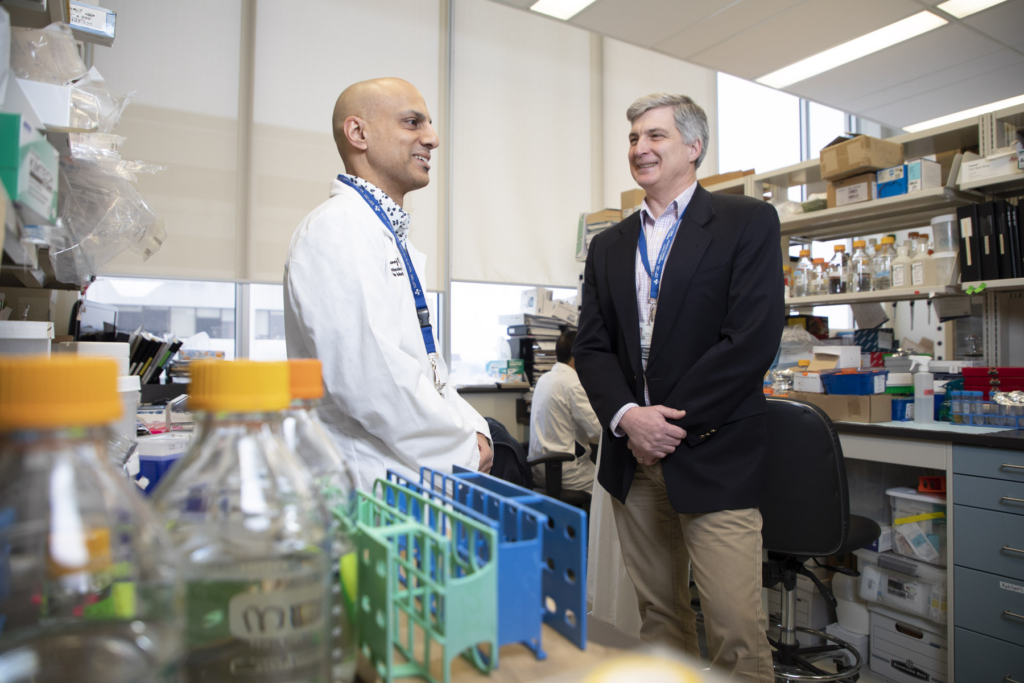
From there, Danika was referred to The Ottawa Hospital’s Rose Ages Breast Health Centre at the General Campus where she met with surgeon Dr. Lisa Findlay-Shirras.
The good news for Danika was her breast cancer was in an early-stage. But because she was so young, that brought other aspects for the care team to consider.
“She went through genetic testing, which we do for many of our younger patients. Thankfully that was negative,” explains Dr. Findlay-Shirras. “We removed the tumour and she chose to have a mastectomy, to avoid the need for radiation, and then breast reconstruction, which is often the choice for a lot of our younger patients.”
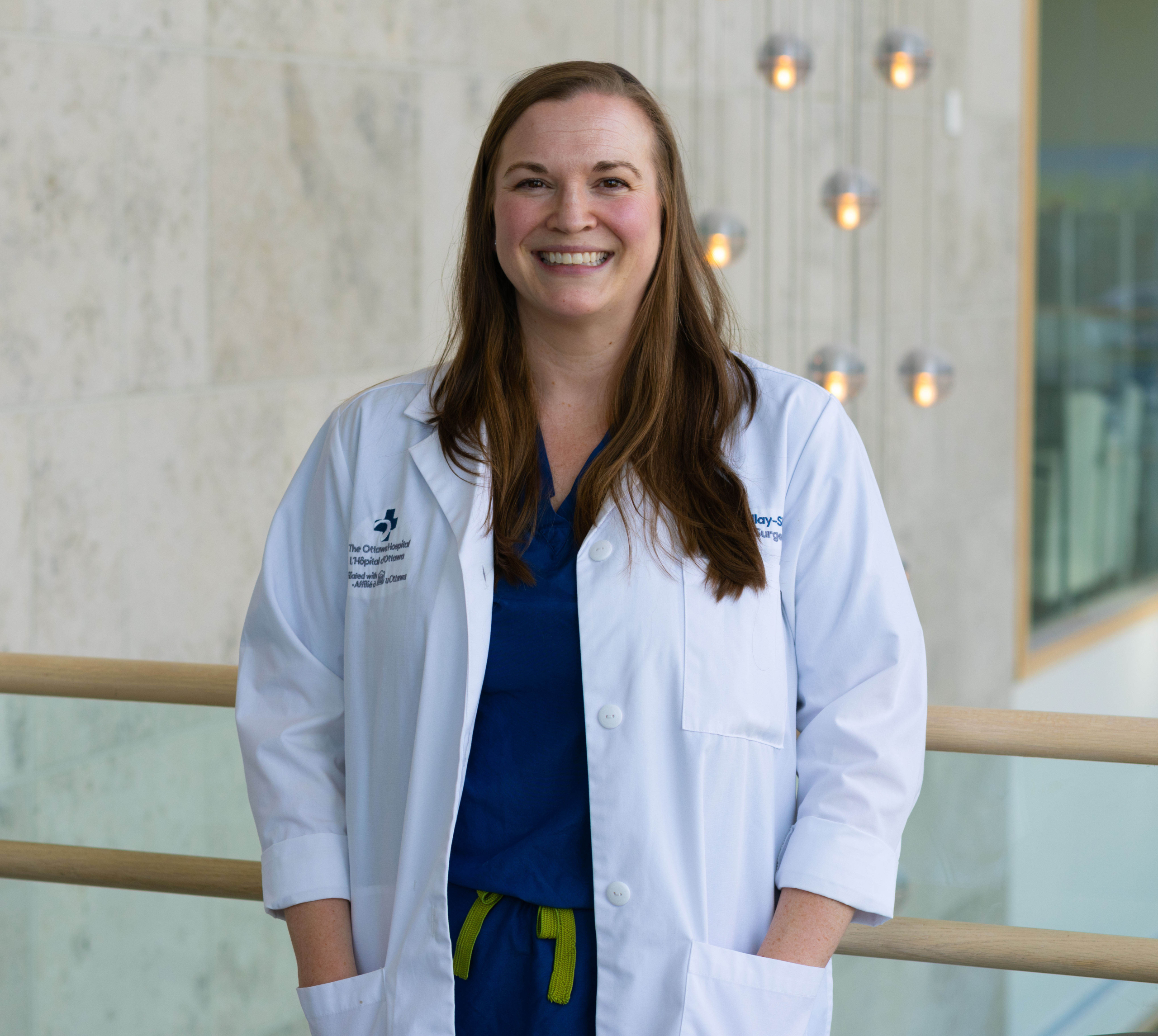
Helping young women navigate through cancer and fertility
Another important factor for young patients is their family planning. “We don’t want a patient, like Danika, to get pregnant for a couple of years when it’s a hormone sensitive tumour where the risk of recurrence is highest. I remember that being a really difficult recommendation for Danika to reconcile,” adds Dr. Findlay-Shirras.
The Ottawa Hospital has a new program, started by medical oncologist Dr. Amirrtha Srikanthan, especially for young women. According to Dr. Findlay-Shirras these patients require a different approach because they have to make difficult discussions about fertility.
“If you haven’t had your family yet when you get diagnosed with breast cancer, it’s reconciling the future you had envisioned for yourself and how it might be affected, and potentially not possible, because of breast cancer treatment. And that’s something you must grieve, which is really hard. So, having resources that are specific to young women is essential.”
Newly married, and ready to start a family, this was difficult for Danika. Due to her breast cancer diagnosis, she had to stop taking birth control pills because the hormones involved can lead to potential recurrence. That’s when she developed symptoms of endometriosis. “I had painful periods and ovarian cysts from a young age. In my 20s, severe pelvic pain led my gynecologist to suspect endometriosis and put me on continuous birth control to suppress my symptoms,” explains Danika. “When I stopped, the endometriosis reared its ugly head and my symptoms became debilitating, setting off a wave of new referrals, tests, and ultimately another surgery.”
What is endometriosis?
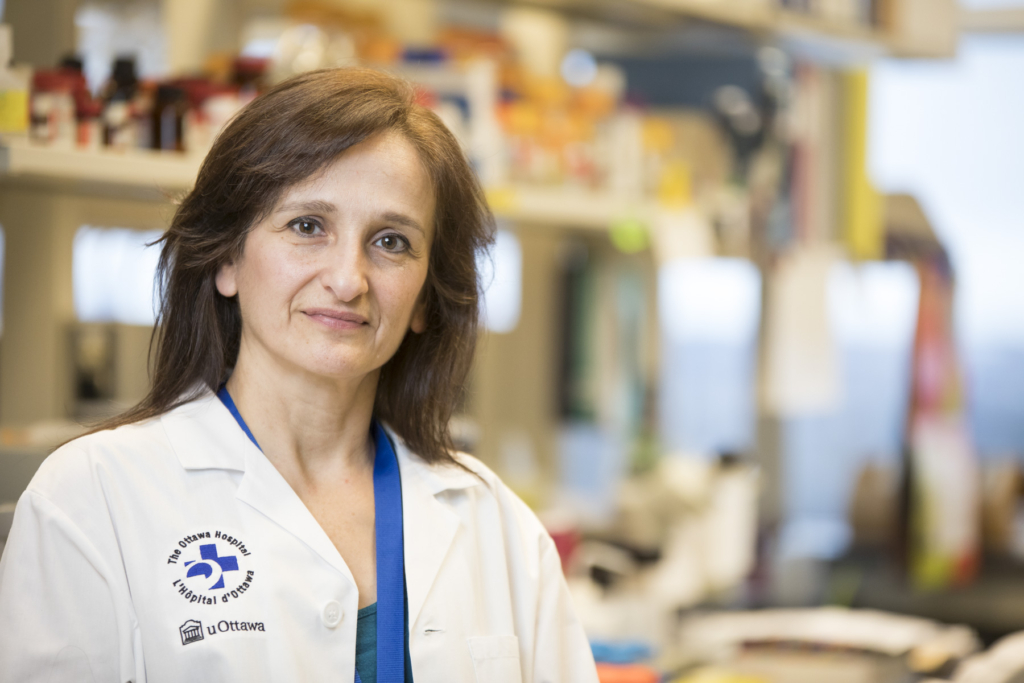
Dr. Sony Singh, surgeon and Head of Obstetrics, Gynecology, and Newborn Care, at The Ottawa Hospital has been advocating for people living with endometriosis for years. It’s a chronic condition where tissue like the lining of the uterus, grows outside the uterus in the pelvic area. It’s often experienced as painful periods and patients are put on the birth control pill or other hormonal medications. While this may reduce the pain, it doesn’t stop the progression of the condition.
“Women are often told their pain is normal and they should live with it. There’s still a lot of misunderstanding and confusion about the disease,” says Dr. Singh.
Meet Dr. Sony Singh
It’s important to recognize that not all women want to be on hormones and some can’t be, like Danika after a breast cancer diagnosis. That’s when the team at the Shirley E. Greenberg Women’s Health Centre needs to look into alternatives, such as non-hormonal treatment options and/or surgery. Surgery, in complex cases, requires an interdisciplinary team with advanced expertise. “The Ottawa Hospital’s endometriosis expertise is nationally recognized as one of the best,” says Dr. Singh.
Danika’s case was certainly a standout to Dr. Singh and his team. “This is one of the most complex cases that I, and our hospital, has ever done for endometriosis.”
All endometriosis
Planning a complex endometriosis surgery
What many don’t know is endometriosis can go beyond the pelvic area and invade other organs such as the bowel, the bladder, ureter, and the kidneys. In Danika’s case, Dr. Singh credits Dr. Kelly Harper, a diagnostic radiologist, who has specialized training in this area, for conducting advanced imaging and determining that Danika’s endometriosis had invaded into the pelvic nerves, which support muscle function, and the ability to walk and move.
"Advanced radiology imaging for endometriosis is something we’re well known for.”
— Dr. Sony Singh
“For the first time at The Ottawa Hospital, we have an expert who’s able to tell me that it’s invading the pelvic nerves and that’s an amazing step for us and our patients. Advanced radiology imaging for endometriosis is something we’re well known for,” says Dr. Singh.
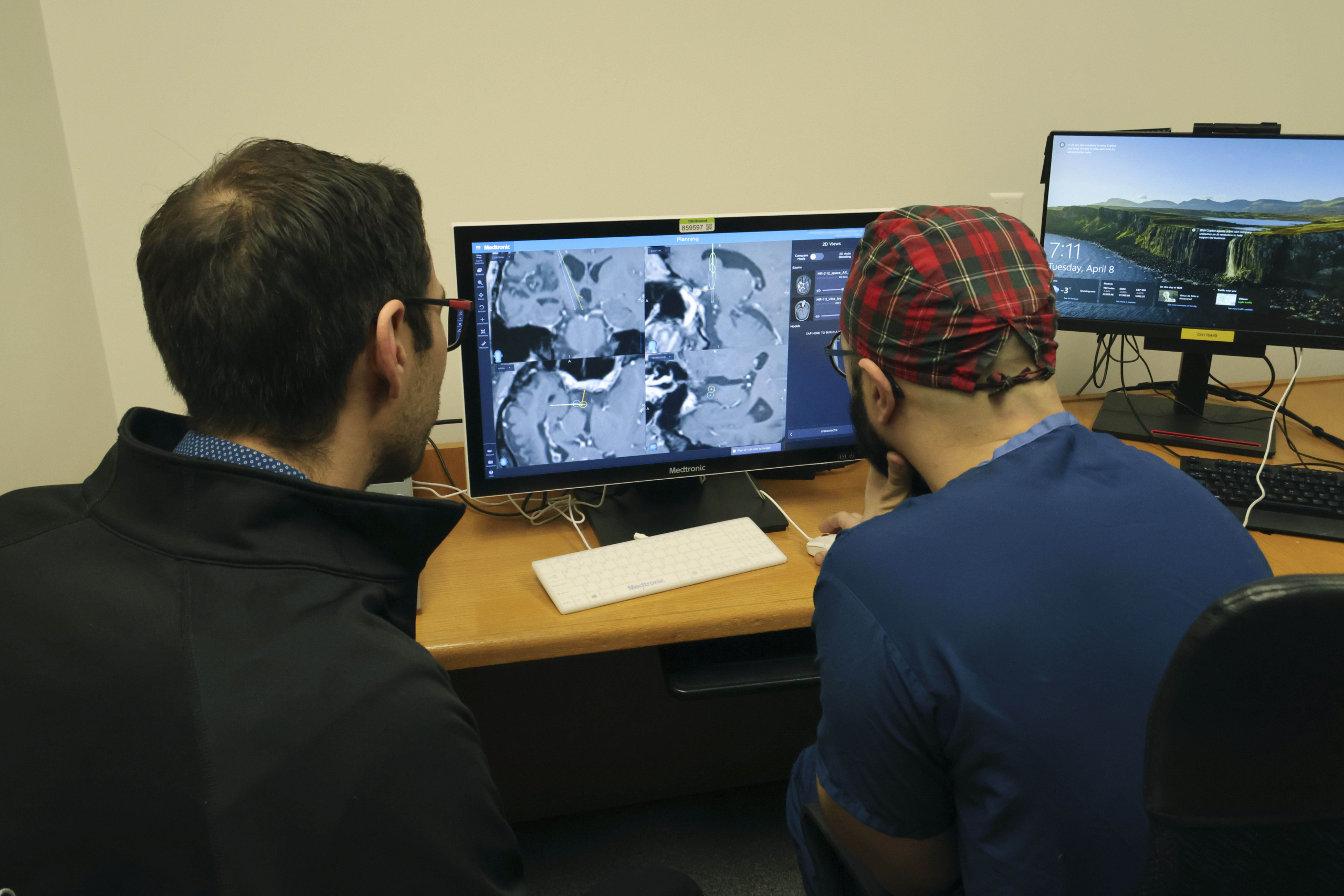
Not only was the team able to identify what was causing all the pain for Danika, but there is also a research program that does virtual reality (VR) through a hospital start-up known as Realize Medical. They created a VR model of the pelvis to not only give this young woman a better understanding about how the disease was impacting her, but also to help the team prepare for surgery.
“All of this together provides this individual with care close to home — patients who would have otherwise had no options or had to travel outside the country to get this care,” adds Dr. Singh.
“This is a complex pelvic-neurosurgery and we’re conducting top-level prep for complex women’s health that has been limited to a few institutions globally.”
— Dr. Sony Singh
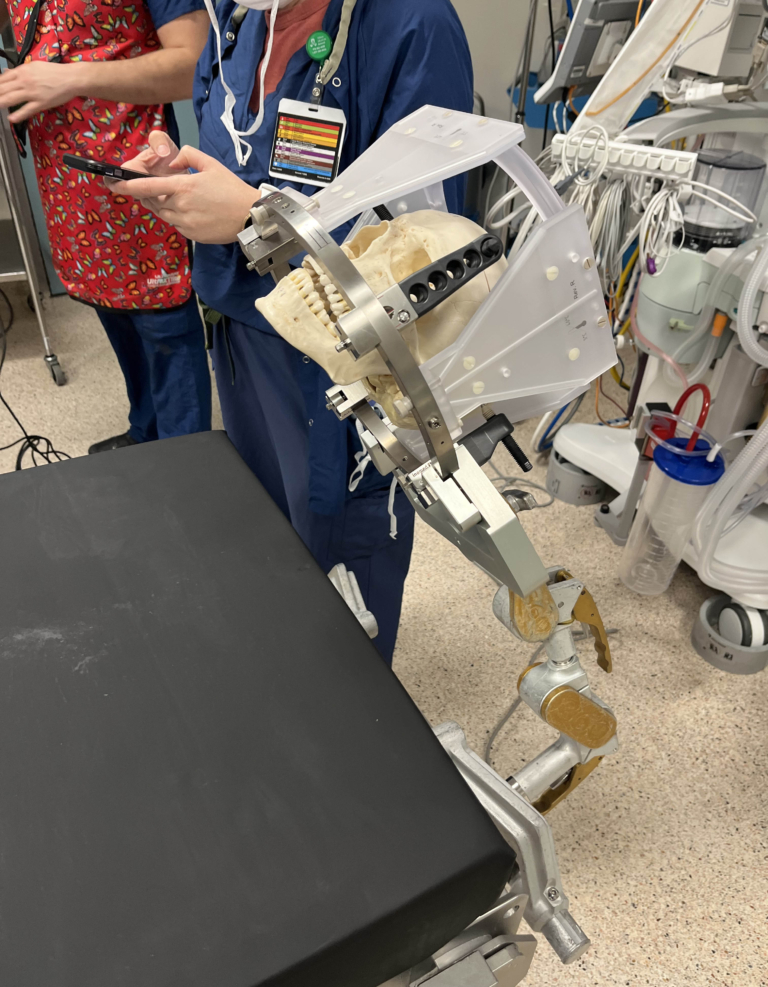
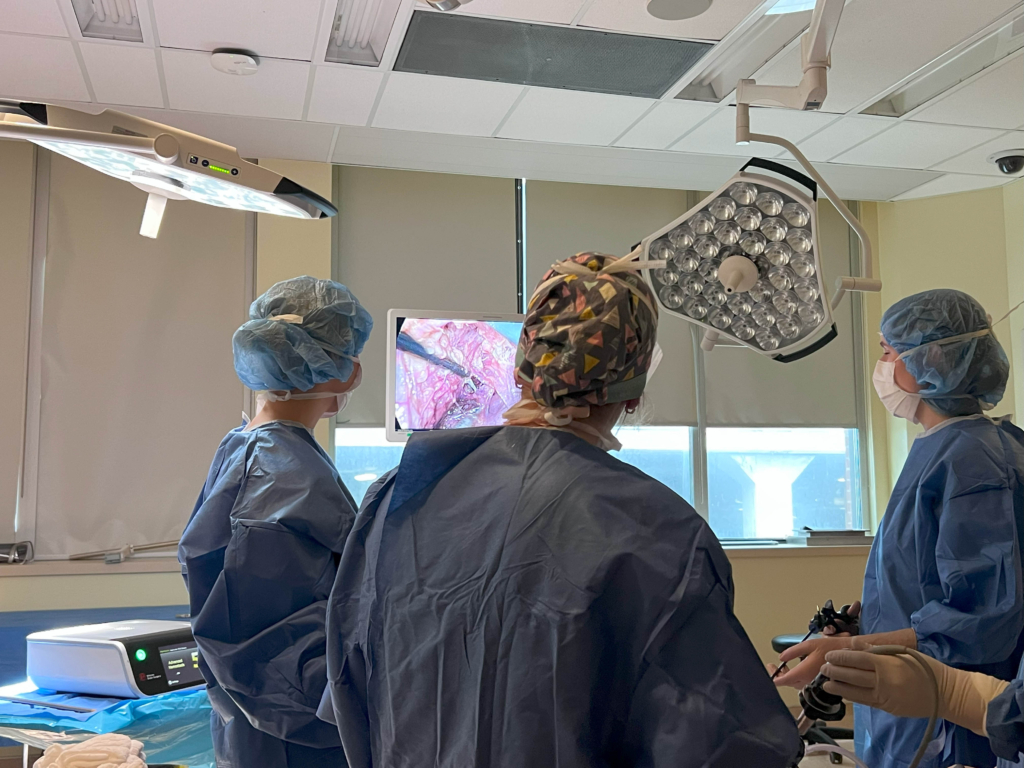
The University of Ottawa Skills and Simulation Centre at the Civic Campus is where Dr. Singh brought together his team in advance of Danika’s surgery. Dr. Singh explains that thanks to the VR model, they were able to simulate the surgery and understand exactly what would happen in the operating room. “This is a complex pelvic-neurosurgery and we’re conducting top-level prep for complex women’s health that has been limited to a few institutions globally”
“Every single person that I interacted with during my care was so lovely, warm, and kind. They were very respectful of me as a person and my wishes and really took the time to understand what was important to me.”
— Danika Fleury
Since the surgery in early September 2025, Danika continues to be cared for by two specialized teams at The Ottawa Hospital. “I’m healing well and already feeling significant relief from pain. I can’t thank Dr. Singh and his team enough for their care, expertise, and use of advanced technology in managing my complex surgery. They have preserved my mobility, restored my overall wellbeing and reproductive health, and most importantly, given me hope, and the chance to get back to living my life fully.”
While she never expected this intensive type of medical care at her age, she’s grateful to each care provider who has helped her along the way.
“Every single person that I interacted with during my care was so lovely, warm, and kind. They were very respectful of me as a person and my wishes and really took the time to understand what was important to me.”
For Dr. Singh, he’ll continue to advocate to ensure more people understand there is hope. “The Shirley Greenberg Women’s Health Centre is a centrer of excellence for endometriosis. We have hired a triage nurse who helps triage all the referrals from family doctors. The more people know, the more we can help these women who have suffered for too long.”