Updated: February 2024
Nearly three years after undergoing groundbreaking immunotherapy for stage 3C colorectal cancer at The Ottawa Hospital, Haydn Bechthold is making strides — he’s currently in his second year of law school in Toronto and will spend another summer at Emond Harnden, a law firm that has supported our President’s Breakfast.
Published: October 2022
As a young athlete playing semi-pro soccer overseas and going to school, Haydn Bechthold admits he felt invincible. But a diagnosis of colorectal cancer at age 22 quickly changed that perspective. The news was a shock, not only to Haydn but also to his family and friends. He was young, active, and otherwise healthy, so a diagnosis of stage 3C rectal cancer was hard news to digest. “I remember thinking ‘Don’t Google survival rates,’” recalls Haydn.
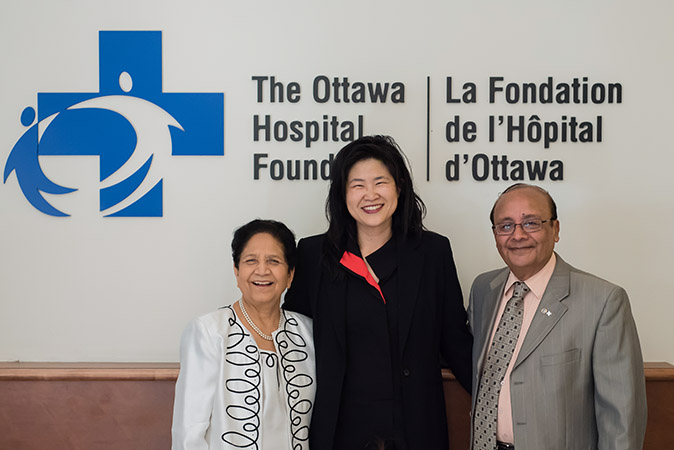
When Haydn was referred to The Ottawa Hospital Cancer Centre, there was a full team assembled. He met with medical oncologist Dr. Joanna Gotfrit, followed by radiation oncologist Dr. Jenny Jin, and surgical oncologist and Director of Cancer Research, Dr. Rebecca Auer. He learned there was some good news — the cancer hadn’t spread.

Dr. Joanna Gotfrit is a medical oncologist at The Ottawa Hospital.
Dr. Jenny Jin is a radiation oncologist at The Ottawa Hospital.
Dr. Rebecca Auer is the Executive Vice-President of Research and Innovation at The Ottawa Hospital and CEO and Scientific Director at The Ottawa Hospital Research Institute
A most unusual case of colorectal cancer
For Dr. Gotfrit, the first thing she remembers after learning about Haydn’s case was how unusual it was to have a patient his age with this kind of a diagnosis — typically, patients are decades older. “No matter the age, whether it’s a very young patient or someone who’s elderly, it’s never easy to deliver bad news. But there is an extra layer and challenge when patients are that young. It’s life-altering, no matter how the trajectory goes,” explains Dr. Gotfrit.

When Dr. Auer left the exam room after meeting Haydn for the first time, she remembers feeling heartbroken, thinking about this young man’s life, his future, and the diagnosis he faced. The standard form of treatment for Haydn was radiation, chemotherapy, and surgery — each one would impact his life. He faced infertility, life with an ostomy bag, and the likelihood of recurrence. “That was hard, but having access to cutting-edge care, we quickly started to think outside the box. I called Drs. Gotfrit and Jin, and we decided to get molecular testing on his tumour,” explains Dr. Auer.
“We knew there was a strong chance we were going to find some rare molecular alterations in his tumour that may drastically change how we would want to approach this case.”
– Dr. Joanna Gotfrit
Those molecular markers from testing would be key to determining the path forward for Haydn’s treatment. Dr. Gotfrit explains while they had the diagnosis and knew the stage of his cancer, there were still underlying questions. “We knew there was a strong chance we were going to find some rare molecular alterations in his tumour that may drastically change how we would want to approach this case. And when I say that, I mean, it may open other avenues of treatment for him.”
Those molecular markers from testing would be key to determining the path forward for Haydn’s treatment. Dr. Gotfrit explains while they had the diagnosis and knew the stage of his cancer, there were still underlying questions. “We knew there was a strong chance we were going to find some rare molecular alterations in his tumor that may drastically change how we would want to approach this case. And when I say that, I mean, it may open other avenues of treatment for him.”
Navigating through the cancer journey
As Haydn and his family came to terms with the diagnosis and attended a multitude of tests and appointments, there was one constant: Mary Farnand — his nurse navigator.
A nurse navigator is a specialized oncology position. Mary works in the Cancer Assessment Clinic (CAC), and along with other nurse navigators at our hospital, is the first point of contact for patients who are being diagnosed. “We review the patient’s history, and initiate some of the work-up, such as bloodwork and scans, to make sure it goes as fast as possible and is personalized,” explains Mary.
“It’s a very difficult time in their life. Our role is to try and provide clarity as well as emotional support.”
– Mary Farnand
The CAC provides a central source of information, support, and advocacy for patients. “We receive referrals, review them, and try to understand what the patients need. We help patients manage symptoms, and if they live farther away, can we direct their scans to another hospital closer to home. We are that source of consistency for each patient,” explains Mary.
This role quite literally helps the patient and their family move through the cancer program and better understand what lies ahead. “We navigate with the patient, giving them as much information as possible to help inform their treatment decisions. It’s a very difficult time in their life. Our role is to try and provide clarity as well as emotional support,” says Mary.

Haydn and Mary Farnand at The Ottawa Hospital’s President’s Breakfast.
Photo by Ashley Fraser.
The CAC provides a central source of information, support, and advocates for patients. “We receive referrals, review them, and try to understand what the patients need. We help patients manage symptoms, and if they live farther away, can we direct their scans to another hospital closer to home. We are that source of consistency for each patient,” explains Mary.
This role quite literally helps the patient and their family move through the cancer program and better understand what lies ahead. “We navigate with the patient, giving them as much information as possible to help inform their treatment decisions. It’s a very difficult time in their life. Our role is to try and provide clarity as well as emotional support,” says Mary.
Haydn is adamant he couldn’t have done any of this without her. “She was such a huge help and so kind to me through this whole process. I remember having so many people contacting me early on and it was quite overwhelming, but Mary was always there. She was always willing to help me figure out what my next move was going to be. She was my constant source of support.”
That support would continue as Haydn’s team got a clearer picture of what kind of tumour they were dealing with.
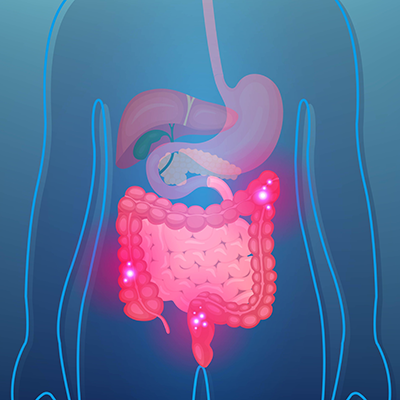
When should I be tested for colorectal cancer?
People who have an average risk of colon cancer should start getting screened regularly at 50. For those with a higher risk — due to family history, a personal history of chronic inflammatory bowel disease, or other risk factors — it might be recommended to get screened earlier or more often.
Early signs of colon cancer include: persistent changes in bowel habits (unusual diarrhea or constipation), rectal bleeding or blood in stool, persistent abdominal discomfort, a feeling of incomplete bowel movements, weakness or fatigue, and/or unexplained weight loss. If any of those symptoms appear alone or together and persist, seeing a doctor is recommended.
Molecular Oncology Diagnostics Lab plays a key role
Further testing helped the care team plan the best course of treatment for this young man. Some of that testing happened at The Ottawa Hospital’s Molecular Oncology Diagnostics Lab — a first-of-its-kind in Ottawa.
The donor-funded lab is revolutionizing cancer diagnosis and treatment by allowing healthcare providers to analyze the genetic flaws inside tumour cells and tailor therapies to a patient’s individual type of cancer. This improves cancer care by giving care teams the ability to predict which drugs would work best for that particular patient’s illness and which drugs would not be beneficial.
Research conducted in the lab gives patients access to the latest experimental cancer therapies before they are available elsewhere. It’s the third lab of its kind in Canada to use the most advanced genetic analysis technology — next-generation sequencing — to analyze patterns from large groups of genes or proteins. The end goal is to improve the detection and control of cancer with more precise treatments customized for each patient.

Haydn and Dr. Auer at The Ottawa Hospital’s President’s Breakfast.
Photo by Ashley Fraser.
“Haydn got this cutting-edge treatment about one year before the world knew anything about it. This was because we have a highly knowledgeable and courageous team that decided to think outside the box for a 22-year-old with cancer.”
– Dr. Rebecca Auer
As Haydn’s team awaited the results of his testing, he was prepping for radiation which was set to begin in March 2021. But as the day approached for his first treatment, he got a call that would change everything. “It was a conference call unlike any I’ve ever experienced. All three of my doctors were on the line. They explained biomarker testing on my tumour showed I had what’s known as MSI-H cancer, which meant I was eligible for a certain type of immunotherapy treatment,” recalls Haydn.
This unique sub-type of rectal cancer has responded well in clinical trials to immunotherapy. As the team explained to Haydn and his family, they used data from the literature to come up with an individualized treatment plan — one they believed would give him the best long-term outcome. “Haydn got this cutting-edge treatment about one year before it was widely known. This was because we have a highly knowledgeable and courageous team that decided to think outside the box for a 22-year-old with cancer,” explains Dr. Auer.
Testing also revealed Haydn had Lynch syndrome — an inherited condition that increased his risk of certain cancers, including colorectal cancer. These test results were valuable information that allowed his care team to develop a personalized treatment for his unique case. They believed immunotherapy would give Haydn the best chance to live a long, healthy life.
The hope of immunotherapy
When Haydn was presented with this alternative to the standard of care, he was excited, but also nervous. “While I was nervous to try something new and futuristic like this, I was also excited by the hope immunotherapy offered me. My family and I had complete faith in my doctors, knowing they could access this treatment, which had been successful in very early studies,” says Haydn.
“The scan showed my tumour had shrunk by almost half. It was incredible.”
– Haydn Bechthold
For Dr. Gotfrit, being able to offer Haydn this treatment option was a game changer. She recalls just eight to 10 years ago, as an internal medicine resident rotating through oncology, there was very little personalized medicine. However, that is changing rapidly. “More and more data, discoveries, and developments about the molecular basis of tumours are coming to light. And, importantly, drugs that could directly target those molecular alterations are being developed. So instead of chemo that essentially ‘shoots to kill’ any rapidly dividing cells in a very nonselective way causing a multitude of side effects everywhere in the body, we’re now developing therapies that are much more selective and can directly target specific mutations in tumours. Being able to identify these molecular alterations is a huge step forward for oncology, giving us more options with a better quality of life. So, it’s a win on all accounts.”
On April 1st, 2021, Haydn started immunotherapy treatment. Within a month of treatment, all of Haydn’s symptoms were gone. No more blood in his stool, no more pain, his energy was back, and he was no longer losing weight.
What is immunotherapy?
Cancer immunotherapy, or immuno-oncology, is a treatment that harnesses a patient’s own immune system to fight their cancer. It works by “training” the immune system to recognize and attack cancer cells, strengthening immune cells to fight cancer, and/or helping the body boost its immune response in other ways. There are many different forms of, and ways to deliver, cancer immunotherapy, including targeted antibodies, vaccines, cell transfers, viral therapies, and more. Cancer immunotherapy is a biotherapy, and it might be used on its own or in combination with other treatments, like surgery, chemotherapy, or radiation.
The news got even better with his first scan two months after treatment began. It was news Haydn was thrilled to hear. “The scan showed my tumour had shrunk by almost half. It was incredible.”
Ready for J-pouch surgery
The immunotherapy treatment continued until July 2021. At that point, the tumour couldn’t be seen on the latest scans and that’s when Dr. Gotfrit called Dr. Auer to say this young man was ready for surgery.By August, a major operation was planned to remove the remaining signs of the tumour and the surrounding lymph nodes. Haydn also underwent a procedure known as J-pouch surgery. This would remove his entire colon to help eliminate any future risk of cancer, while also allowing him to live a normal life without an ileostomy bag. It was during this surgery that Dr. Auer made a remarkable discovery — there were no signs of cancer. “This was a really wonderful moment. Thinking back to the day I met him, and I thought for sure he was going to break my heart, here we were with a really amazing outcome. This was a young man who potentially had his whole future back,” says Dr. Auer.
Once the J-pouch healed, Haydn was back in the operating room in November of 2021, this time with Dr. Shaheer Tadros and Dr. Auer to remove the temporary ileostomy and finish the J-pouch procedure. He was about to get his life back.
How J-pouch surgery works
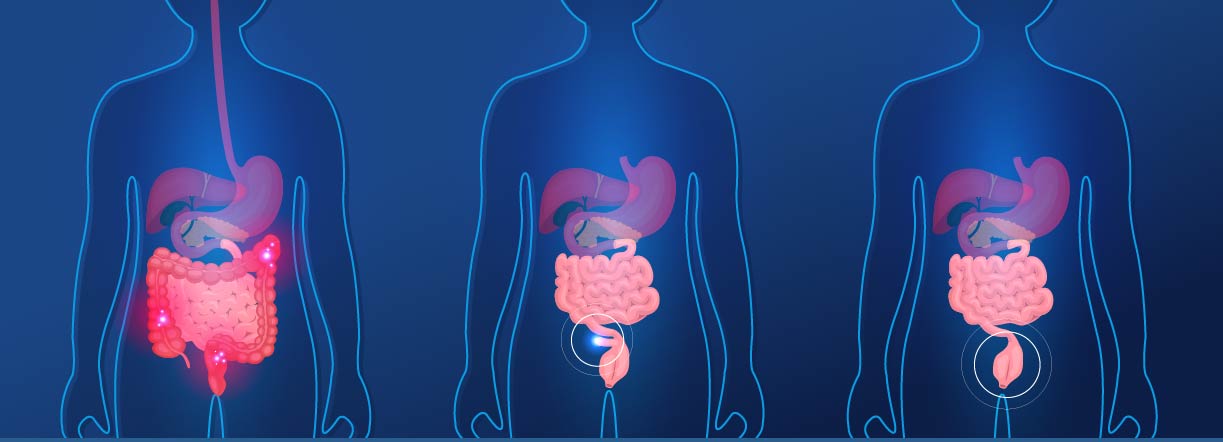
BEFORE SURGERY
- Colon and rectum present
- Patient suffering from symptoms
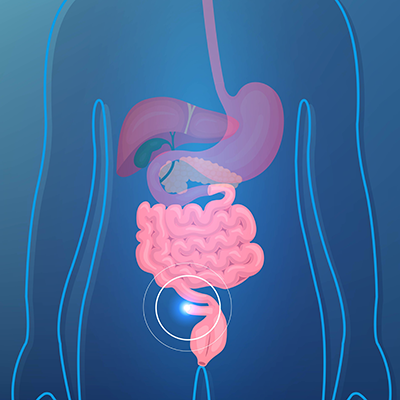
DURING SURGERY
- Colon and rectum removed
- J-shaped pouch constructed from small intestine and attached to anus
- Ileostomy bag placed during surgery to help with the healing of the pouch
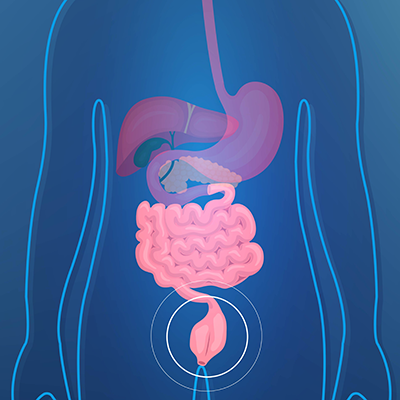
SECOND-STAGE SURGERY
- Ileostomy bag reversed
- POST SURGERY J-pouch and anus fully functioning
The role research plays in changing the course of cancer care
When faced with a challenging cancer case, our cancer experts didn’t settle for the standard of care — knowing the long-term impact it could have on Haydn’s life. Instead, they dug deep and offered him an alternative with better long-term quality of life — immunotherapy treatment.
Since starting her own research laboratory at The Ottawa Hospital in 2007, Dr. Auer has focused on the interplay between cancer, surgery, and the immune system — making many important discoveries. “Surgery is very effective in removing solid tumours. However, we’re now realizing that, tragically, surgery can also suppress the immune system in a way that makes it easier for any remaining cancer cells to persist and spread to other organs.”
Dr. Auer’s team has discovered how this happens and they are now testing different strategies in the lab and in patients to modify the immune system and prevent cancer from coming back after surgery. These trials often include patients with colorectal cancer.
Just a few years ago, Haydn never gave much thought to research, let alone cancer research, but his views are very different today. “There are so many advances every year in this field, especially clinical trials, it’s really exciting. I think a lot of people hear the term clinical trials, myself included when I was in treatment, and are quite scared. But a lot of the time, it’s the most up-to-date or newest form of treatment and possibly the best, so the importance of research is massive.”
Setting his sights on the future
Just a few months after Haydn’s second surgery he started feeling like his old self. He began exercising again and putting on weight. Incredible progress in a very short time after his shocking diagnosis.
Today, Haydn continues to be monitored closely by Dr. Gotfrit, and will be for the next few years, but the cancer is gone and he’s getting back his life. As far as his medical oncologist is concerned, that’s the best possible outcome she could have imagined for him. “This is exactly why you go into medical oncology. It’s the absolute best feeling in the world to put in all that effort, thought, and agonize over what’s the right thing to do for this young man. And then make the best decision possible and see that it worked as well as or better than you ever could have imagined. It’s hard to describe how good that feels,” says Dr. Gotfrit.

Mary Farnand, Dr. Auer, Haydn and his parents at The Ottawa Hospital’s President’s Breakfast.
Photo by Ashley Fraser.
“I also realize how incredibly fortunate I was to have The Ottawa Hospital and this team of doctors who wouldn’t settle for traditional treatments — who thought outside the box to give me the best life possible.”
– Haydn Bechthold
For Haydn, it’s a team effort he won’t soon forget. “I never worried about death before this, but I realized I’m not invincible. I also realize how incredibly fortunate I was to have The Ottawa Hospital and this team of doctors who wouldn’t settle for traditional treatments — who thought outside to box to give me the best life possible. I felt like they all really cared.”
Now living in Toronto and going to law school, you can still find Haydn kicking the soccer ball around for fun, and he says with a smile that he might not be done with soccer yet. Now he has time on his side to make that decision.