Published: May 2023
Sometimes you meet someone and wonder what drew you together. That’s what happened when Holly Wagg met Lynne Strickland in Patagonia, Chile. Both women lived in Ottawa, but it was a serendipitous meeting almost 10,000 kms from home where they ended up as bunk mates while on an expedition. Soon, they would discover a special bond between them — they both had loved ones who faced leukemia, and while their journeys were different, their stories connected in an unexpected way.
The story begins in the fall of 2015 when Holly’s wife, Julia Wagg, started to feel inexplicably tired. At the time, the Director of Talent Management at Hydro Ottawa was also teaching a course at Carleton’s Sprott School of Business, and juggling life with three children — she had a lot on her plate. But then one day she noticed blood in her mouth and decided she’d better make a dental appointment. By early December, symptoms escalated. “Julia woke up at 2 or 3 a.m. one night and said, ‘I need to go to the hospital.’ She could hardly breathe because she had crushing chest pain,” remembers Holly.
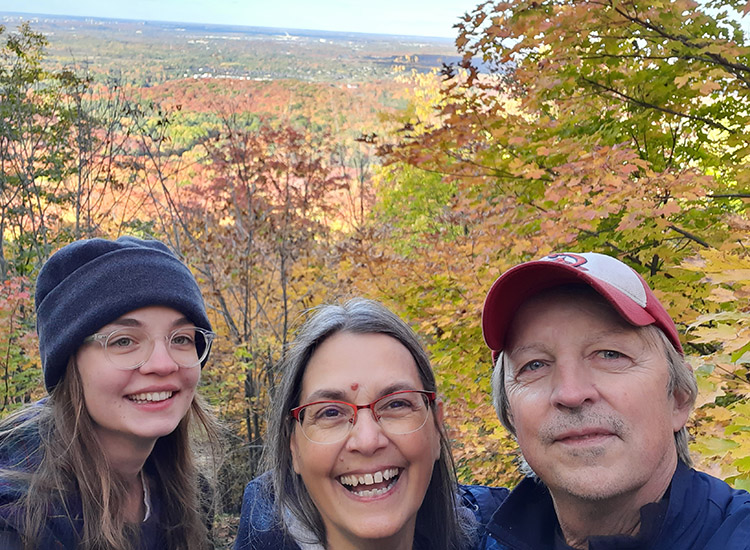
That first visit to the hospital didn’t determine any clear signs of what might be wrong, but Julia’s fatigue persisted into the new year. The family had big plans to travel to Africa, and Julia was determined to go. Holly was leaving early to climb Mount Kilimanjaro, then Julia and their youngest daughter, Addison, would follow two weeks later.
Leukemia diagnosis heard around the world

As Holly summitted the mountain, back home Julia received devastating news. “While I had been up there, she had taken herself to the hospital one morning, and they told her she wasn’t leaving — she had leukemia,” says Holly. “Julia waited four days to tell me so I could finish my climb. When I found out, I raced back as soon as I could.”
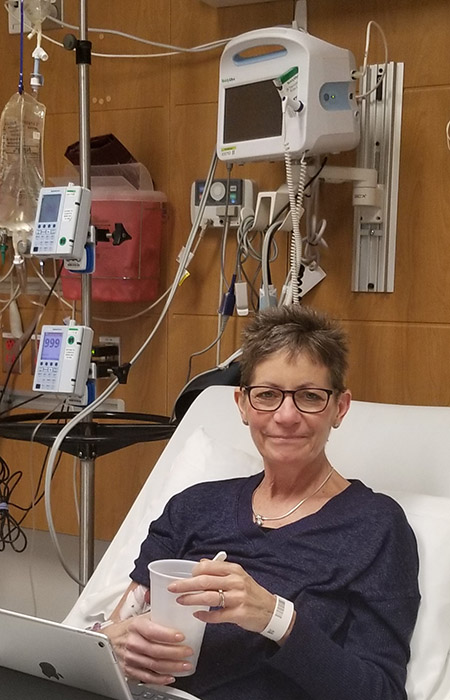
The life Holly returned to was much different than the one she had left. Julia was immediately put on a chemotherapy cocktail — 24/7. She remained hospitalized for three to four weeks and when Holly was finally able to visit her in the hospital, she says the reunion was heartbreaking and devastating. “Julia was going through this fight of her life and was having so many complications from chemo. I was researching and I knew what we were facing.”
The couple learned Julia had the acute myeloid leukemia mutation known as FLT3. It was aggressive. “This is like driving your car and slamming your foot down on a gas pedal — that’s how fast the cancer was reproducing. Most people have a 10% chance of surviving five years,” explains Holly. “So, my mission became to make whatever time we had left the best possible time.”
By the second round of chemo and after 12 weeks as an in-patient, Julia was in remission and was eligible for a stem cell transplant. Her sister was a match, and three weeks later, in May 2016, Julia received the transplant of her sister’s stem cells — and the hope for more time with her family.
However, Julia faced one complication after another and spent the better part of eight months in the hospital. “Her whole team of doctors and nurses up on 5 West and the Bone Marrow Transplant team at The Ottawa Hospital were amazing,” remembers Holly. “She left hospital in December with limited mobility, but started strength training and eventually we had her skiing. We learned how to cross-country ski.”
Making the most of their precious time left together
The family had what Holly describes as the perfect three months of a cancer-free life. During Julia’s cancer care, she never made promises to her children, but there was one exception. She told Addison she would be there to celebrate her sixth birthday — things were going well. A big birthday party was planned with a fairy theme and all their friends came together to celebrate. “It was beautiful and joyous,” remembers Holly.
But after the party, Julia collapsed on the floor in agony from extreme bone pain. By the next day, the same thing happened, and she went to the hospital. The blood work looked normal, so they did a bone marrow biopsy. When Holly and Julia returned to the hospital for the results, Julia couldn’t walk.
Julia’s cancer was back. The couple knew if a patient relapsed within 12 months following a stem-cell transplant, there’s no chance of a second transplant. It had only been 11 months.
Julia passed away in the ICU of The Ottawa Hospital a week-and-a-half later. “She had all the people who loved her around the bed that night. I brought Addi into the room, and I grabbed Harry Potter because that was the story we were reading at the time. As I was reading, Julia’s heartbeat started to decelerate. I wanted to stop, but I knew she needed to hear me. She needed to know we’re all okay,” recalls Holly. “Jules was surrounded by love, and she chose to let go during this beloved bedtime ritual.”

Meeting a ‘spitfire’ young researcher
Before Julia passed away at the age of 36, she and Holly had some difficult but honest conversations. During her lengthy time in hospital, Julia witnessed many things as a patient. As a patient at a teaching hospital, she met many rotations of residents, in both the physician and nursing programs. Julia often said yes to the residents who were taking blood for the first time, and she said yes to two doctors who performed their first bone marrow biopsies. She wanted to help.
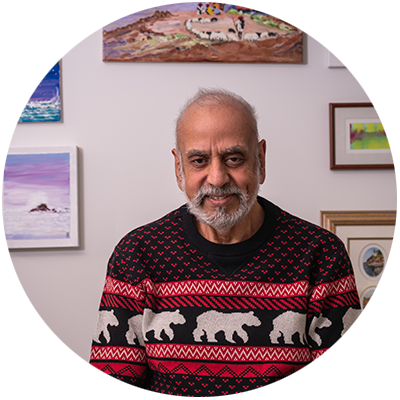
“One of the physicians who cared for her was Dr. Natasha Kekre. She was a spitfire — she was young, and she was brilliant. She was looking to start a clinical trial at The Ottawa Hospital to offer breakthroughs in leukemia treatment using CAR T-cell therapies. Julia wanted to elevate that research.”
– Holly Wagg
Because of the aggressiveness of her cancer, she also interacted with many physicians who were also researchers. “Julia was very curious and asking them about their projects. One of the physicians who cared for her was Dr. Natasha Kekre. She was a spitfire — she was young, and she was brilliant. She was looking to start clinical trial at The Ottawa Hospital to offer breakthroughs in leukemia treatment using CAR T‑cell therapies. Julia wanted to elevate that research,” explains Holly.
Julia and Holly had read about CAR‑T and knew what the possibilities would mean for patients like Julia in the future. It was the first big game changer to leukemia treatment in more than 20 years. They had seen what was happening in the United States and believed patients in Canada should have access to it. “Being a part of research to improve that path for people going forward was very important to both of us, which is why, for us, that legacy was about making sure other families didn’t have to experience what we did. We wanted to be a part of that change,” says Holly.
What is CAR-T therapy?
Julia’s legacy and her commitment to research
With that in mind, Julia decided to leave a gift in her will to support research at The Ottawa Hospital. Her legacy would live on. Holly has also committed to leaving a gift in her will to build on Julia’s wishes and to further fund research that was so important to both of them.
By 2019, The Ottawa Hospital became one of three centres in the province administering the Ontario CAR T‑cell Therapy program for adults — just the type of progress Julia would have wanted. The program meant the T‑cells could be collected from the patient here, then sent to the U.S. to be genetically engineered into CAR T‑cells. Those cells are returned to the hospital and injected back into the patient so they can target and attack the cancer. The challenge is that it’s only available for patients with a specific type of lymphoma and leukemia. Commercial CAR‑T therapy is also very expensive and time-consuming. The commercial cell manufacturing, testing, and shipping process can take up to eight weeks– time that many of the sickest patients don’t have.
What is a legacy gift or an estate gift?
Both terms refer to a donation to a charity made through your will or estate plans. These donations can take several forms, such as cash, securities, or even property.
That wasn’t good enough for people like Dr. Kekre – she wanted to develop a made-in-Canada solution. Today, she’s helping to lead a Canadian-first CAR T‑cell therapy clinical trial at our hospital. This opens the door to faster, less expensive, and more equitable CAR‑T treatment across Canada. It also provides a platform for the development of even better cellular immunotherapies that may work for more kinds of cancer. World-class research facilities at The Ottawa Hospital, such as the Biotherapeutics Manufacturing Centre, have played a key role in the development of this platform.
“It was amazing to get updates on the project because we found out that it was going to clinical trial and there were very positive early results,” says Holly. “And then I saw the first face of a trial participant — a man named Owen. Then I read Camille’s story. And that was an amazing one for me.”
Making the connection
The impact of Julia’s forward thinking became even more personal when Holly had that chance meeting with a stranger in another hemisphere in February 2020. She and Lynne were both seeking adventure in Patagonia. For Holly, it was a big step — the first time she had travelled since Julia’s death. The two women bonded when they realized they had a special connection — Lynne’s daughter, Nicole Strickland, had been diagnosed with acute lymphoblastic leukemia in 2018 and treated at The Ottawa Hospital.
“We had that common kind of understanding of seeing a loved one go through leukemia, the challenges, and a stem cell transplant,” explains Lynne. “But then when Nikki relapsed, I remembered Holly had mentioned Julia’s legacy had gone to funding research into CAR‑T.”

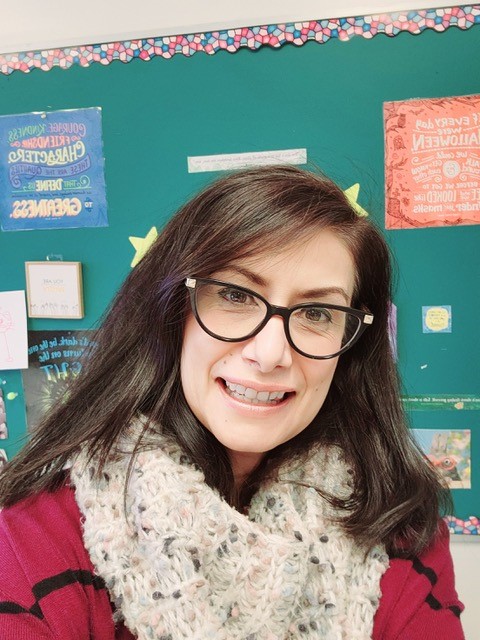
Nicole was just 19 years old and in military college when she was diagnosed. At the time, she was stationed at CFB Petawawa for job experience with the helicopter squadron. She underwent chemotherapy treatment, but because her cancer was aggressive, her care team at The Ottawa Hospital recommended a stem cell transplant. Nicole’s sister was a 100% match. The stem cell transplant took place in September 2018, and then Nicole went into remission.
By the summer of 2021, Nicole was posted with a new unit in Halifax and getting routine blood work. That’s when she learned her cancer was back. But this time, she was introduced to immunotherapy, which she received in Halifax, followed by CAR‑T therapy — which meant returning to The Ottawa Hospital.
“There was a world of difference between CAR T‑cell therapy and the stem cell transplant,” explains Nicole. “I lost 40 pounds during the stem cell transplant. I couldn’t eat. I almost had to get a feeding tube at one point, which scared me. It took me about eight months to fully recover and then another year to get back into the gym. It was also mentally difficult. But with CAR‑T, I had energy, and my spirits were good. There were just a few days of feeling off and then I was back on my feet.”
How CAR T-cell therapy gave Nicole new hope
Nicole qualified for the Ontario CAR T‑cell Therapy program, which saw her T‑cells shipped to the U.S. to be genetically modified into CAR T‑cells. Once they were shipped back to The Ottawa Hospital, they were then infused into Nicole’s body.
“Unless you’ve been through what my family and I have been through, it’s hard to understand the depth that donating to a cause like that means. CAR-T gave me my life back — I’m just so grateful.”
– Nicole Strickland
Today, 18 months after her CAR‑T treatment, Nicole is now an operations officer and continuing her military career in Halifax and feeling stronger each day. She’s deeply grateful to people like Julia who had the forethought to invest in cancer research. “Unless you’ve been through what my family and I have been through, it’s hard to understand the depth that donating to a cause like that means. CAR‑T gave me my life back — I’m just so grateful.”
It’s those who support research that pave the way for patients like Nicole to have better outcomes. For Lynne, it’s also the work that’s came before breakthroughs like CAR-T that is just as important. “For Nikki’s care during the stem cell treatment, they had a plan, and that plan was because of the research and the investment made by others before CAR‑T was an option. It’s about bringing forth solutions that save not just one person’s life, but their whole family,” says Lynne.


“It’s about bringing forth solutions that save not just one person's life, but their whole family.”
– Lynne Strickland
For Holly to make that personal connection with Lynne and to see someone as young as Nicole have success is not something she ever expected. “As a donor, somebody who invests in research, I never expected to see any transformation in my lifetime. I’m willing to wait and be patient. But I never expected to see actual change to medical practice in my lifetime. And never mind did I expect to see it just a few short years after my wife’s death.”
And so, Julia’s legacy continues today, not only through her three children Robin, Brandin, and Addison, but also through the research she helped fund — research that is changing the course of cancer care. The more faces Holly connects back to the research and the more stories of survival she learns about, the more she witnesses Julia live on. “When you think about a legacy and about what you leave for others and how you shape a world — how much more powerful can that be knowing that in some way you’ve given other people an extra shot at life?”