For months, Mina King had been dealing with painful leg ulcers caused by atherosclerosis, a condition that restricts blood flow and can result in amputation if left untreated. As a lifelong musician, this prognosis would mean more than losing her legs, it would jeopardize her ability to play the piano — one of her greatest passions. But, a cutting-edge surgery technique at The Ottawa Hospital, the collaboration of our experts at the Limb Preservation Clinic (LPC), and ongoing virtual care to monitor her healing, kept Mina from missing a beat.
Ulcers: A persistent problem
When Mina first developed sores on both of her legs, she hoped they would eventually go away with time and care. But after almost a year and a half of appointments and regular monitoring at the LPC, things weren’t heading in the right direction.
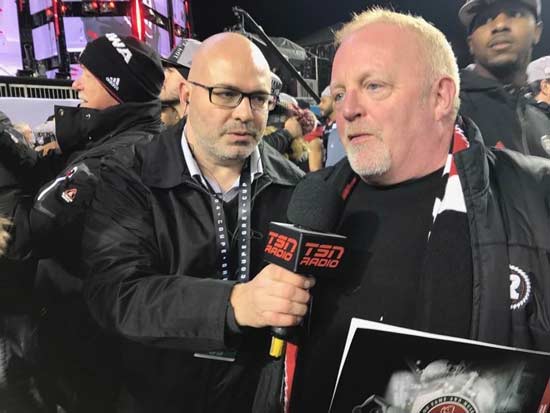
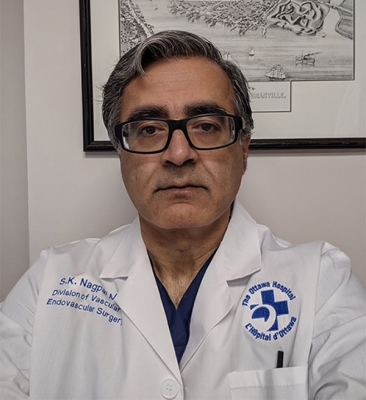
“Bypass surgeries are very complex and take several hours to complete. Not every hospital is able to perform these surgeries because they’re so technically demanding, and the vessels are so small, but The Ottawa Hospital does more of these intricate procedures than any other hospital in Ontario.”
— Dr. Sudhir Nagpal
“Even though I was getting treated for my leg ulcers, they didn’t improve in size or seem to get any better. And they were painful too,” says Mina, an 89 year old retired music teacher and lifelong musician.

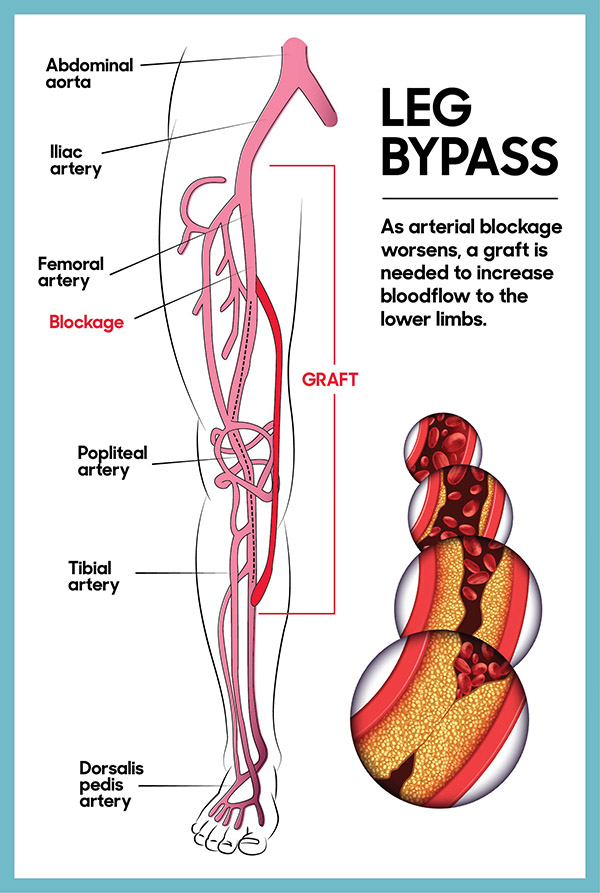
Mina’s ulcers were caused by atherosclerosis, a condition where an artery’s blood circulation is slowed because of plaque buildup. While the condition is commonly caused by diabetes, it can also develop with age. Without medical attention, the ulcers can worsen, causing infections or risk of losing a limb.
“If Mina’s leg ulcers worsened, we would have to amputate her legs to save her life,” says Dr. Sudhir Nagpal, division chief of vascular surgery at The Ottawa Hospital and surgeon in Mina’s care. While it would save her life, a double amputation would mean Mina could no longer use the foot pedals of her piano — which she plays every day. “It’s been the strength of my life to be able to play the piano,” says Mina. “I knew something would have to be done.”
After a CT scan in 2020 revealed blood clots had formed in both of Mina’s legs, her care team decided it was time to take action.
Bypassing the blockage
Luckily, Mina’s ulcers hadn’t progressed to the point where she needed full amputations and surgery was still a viable option.
In August 2020, surgeons and interventional radiologists at our hospital were able to perform a minimally invasive surgery on her right leg, placing a stent in the artery, to improve blood flow and keep the artery open. However, this approach didn’t work for her other leg.
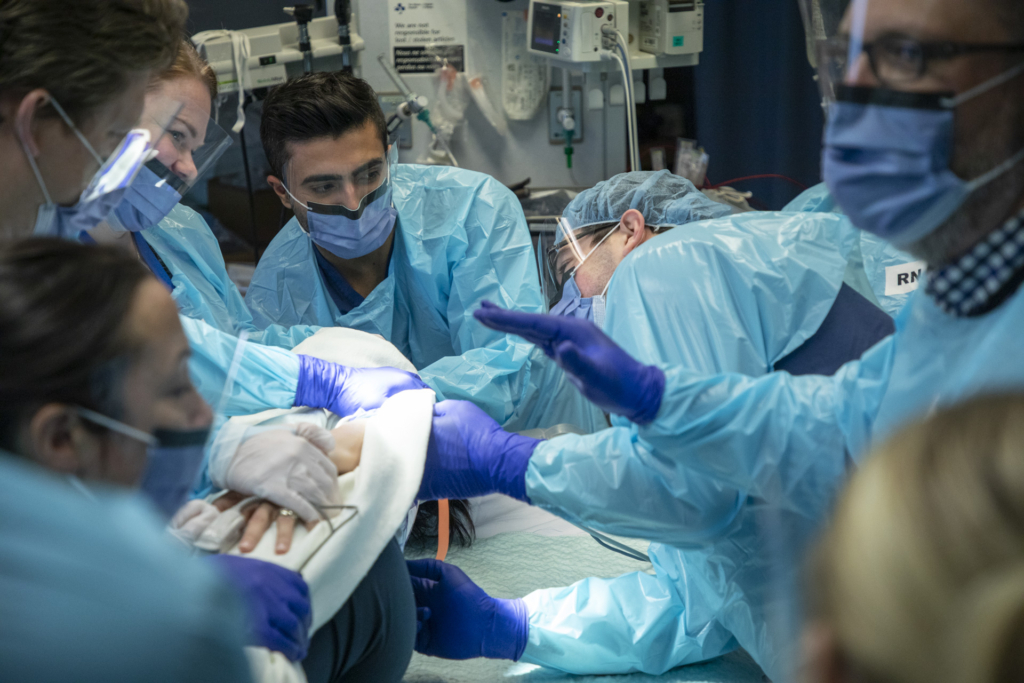
To get blood flowing in her left leg, surgeons performed a complex leg artery bypass surgery, rerouting her blood supply around the blocked artery with a graft – like a road detour. During Mina’s nearly five hour procedure, a team of highly-skilled experts in vascular surgery used magnifying glasses to carefully connect Mina’s vein around the blocked artery, above and below the obstruction, to create a new route for blood to flow.
Thankfully, Mina had access to this specialized surgical technique at our hospital — a procedure not available everywhere.
“Bypass surgeries are very complex and take several hours to complete. Not every hospital is able to perform these surgeries because they’re so technically demanding, and the vessels are so small, but The Ottawa Hospital does more of these intricate procedures than any other hospital in Ontario,” says Dr. Nagpal.
Identifying a safer anesthesia option – thanks to research
At the time of Mina’s surgery, our researchers had just wrapped up a study on anesthesia and leg artery bypass surgery. The study, which was published in The British Medical Journal in November 2020, showed that patients who had surgery to improve blood flow in their legs fared better and were able to leave the hospital earlier if they had lighter forms of anesthesia, such as epidural anesthesia, that don’t require a breathing tube.
“We’re able to provide excellent, nation-leading clinical care because of the experts we have access to and the research happening right here in the clinic at The Ottawa Hospital.”
— Dr. Sudhir Nagpal
Because Mina’s surgeons had early access to the study’s results at the time of her procedure, they were able to recommend that she opt for the epidural anesthesia. “They asked me what kind of anesthesia I wanted to have and described the different ones but suggested that being 89, it would be safer to get the epidural,” says Mina. “And it all went really smoothly.”
According to Dr. Nagpal, having this research happening under our roof is critical. “Mina was able to benefit from some of the research we’re doing and have a better outcome.”
Access to world-class care
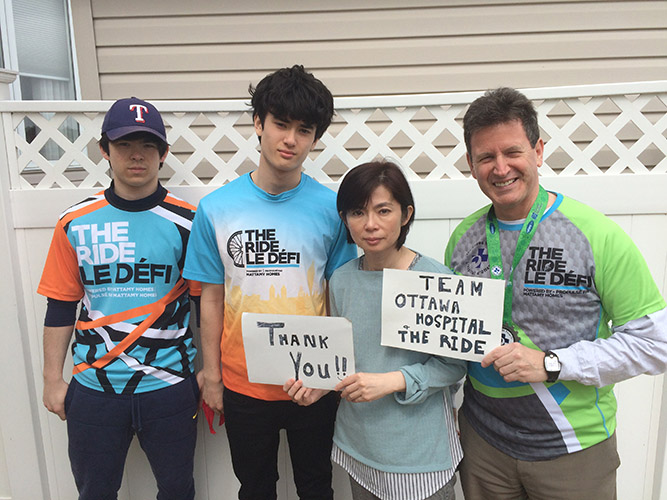
Despite the complexity, Mina’s surgeries were a success. But her path back to the piano wasn’t over yet. One week after her surgery, Mina was discharged to continue her recovery at home with the help of virtual care through the LPC.
The clinic, which began as a pilot project several years ago, brings together care providers from across our hospital with expertise in lower-body wounds. While in the clinic’s care, patients like Mina have access to experts in vascular surgery, wound care, plastic surgery, infection prevention and control, orthopedics, chiropody, and more. The model of care means that patients can access the experts they need without long delays. In fact, it’s a model that hospitals across the country are looking to follow.
“The collaboration between multiple different skill sets and specialties all in one place is what really separates our Limb Preservation Clinic from others like it in Canada,” explains Dr. Nagpal. “We’re able to provide excellent, world-class clinical care because of the experts we have access to and the research happening right here in the clinic at The Ottawa Hospital.”

Mina’s care team tracked the progress of her ulcers through a wound care software called how2trak. With the help of an at-home nurse who made weekly visits to Mina’s home following her surgery, photos of Mina’s leg wounds were uploaded into the software and analyzed by her care team to determine if the wound was getting better or worse over time.
“Through this software, we’re able to see that Mina’s ulcers have gone from being fairly large in size to the point where they’re almost healed,” says Dr. Nagpal. “We can do all this while she’s in the comfort of her home.”
Back at the piano
As Mina’s condition improved, her visits with the at-home nurse and experts in the LPC became less frequent. “I feel quite happy about the way things have gone. I don’t have pain now,” says Mina. “Dr. Nagpal was an excellent doctor.”
“It’s been the strength of my life to be able to play the piano.”
— Mina King
Now, with her ulcers nearly healed and access to the expertise of her care team just a virtual call away, Mina is back to her routine of playing the piano every day — without worry.
“I was very glad to get back home and get back to my piano. I think it was one of the things that helped me recover so quickly,” she says. “When I get tired, or anything’s bothering me, I sit down at the piano and it seems to just take it all away.”
The Ottawa Hospital is a leading academic health, research, and learning hospital proudly affiliated with the University of Ottawa.