The Ottawa Hospital has made great strides in addressing today’s most pressing challenges in neuroscience. We are internationally recognized for our groundbreaking research and treatment of many neurological diseases, such as stroke, neuromuscular illnesses, and Parkinson’s disease (PD).
In fact, we are one of very few centres in Canada where neurologists work hand-in-hand with basic scientists to tackle unsolved problems. Our goal is to foster new ideas and expand our range of clinical trials to quickly bring cutting-edge treatments directly to our patients. Some of the discoveries that lead to new interventions have been made here.
Parkinson’s disease is the second most common neurodegenerative disease after Alzheimer’s, affecting over 100,000 Canadians. The disease continues to mystify according to Dr. Michael Schlossmacher, a neurologist and the Bhargava Family Research Chair in Neurodegeneration at The Ottawa Hospital. This Chair is an example of one way philanthropists, like the Bhargava family, actively support the hospital.
“It was in 1961 when one of my teachers in Vienna first discovered the Lazarus-type effect of how dopamine therapy can suppress the symptoms of Parkinson’s. That was six decades ago, and we now understand more of the mechanisms underlying the motoric deficits, but we still don’t have a therapy in place to stop the illness in its tracks,” says Dr. Schlossmacher.
Thinking outside the box for Parkinson’s treatment

“If we want to treat Parkinson’s, slow it down or stop it, it will only happen through research that identifies better ways to separate subtypes of the illness and confirm targets to develop drugs for interventions.”
– Dr. Michael Schlossmacher
While progress is slow and often frustrating for patients, active research continues to probe for answers. “If we want to treat Parkinson’s, slow it down or stop it, it will only happen through research that identifies better ways to separate subtypes of the illness and confirm targets to develop drugs for interventions. Then, we’ll need to test them in the clinic and, upon demonstration of safety, apply them to a large body of patients in trials to gauge efficacy,” explains Dr. Schlossmacher. He is quick to point out that our Parkinson’s Research Consortium has made a name for itself in Canada and internationally, both on the clinical side and through basic research. Some of the clinical research activity is directed at improved integration of care delivery that we have already available today.
Philanthropy and grants play a pivotal role in moving research forward. For Dr. Schlossmacher and his team, it often allows them the opportunity to develop ideas that are largely out of the mainstream and represent ‘outside the box’ thinking. “Philanthropy has the potential to transform research activities by amplifying them and supporting talented trainees that can work on creative, new ideas.”
Does Parkinson’s start in the nose?
Over the years, research has shown more than 80% of people with Parkinson’s disease suffer from a reduced sense of smell — it often occurs years before the onset of typical movement-related symptoms. Understanding those early indicators could help in an early diagnosis for patients.
Recently, a US $9-million grant from the Aligning Science Across Parkinson’s (ASAP) initiative was announced to further explore this idea. The hope is to determine whether scent-processing nerves that connect the inside of the nose to the brain may play a role in the development of the disease. Dr. Schlossmacher is the overall leader of the effort.
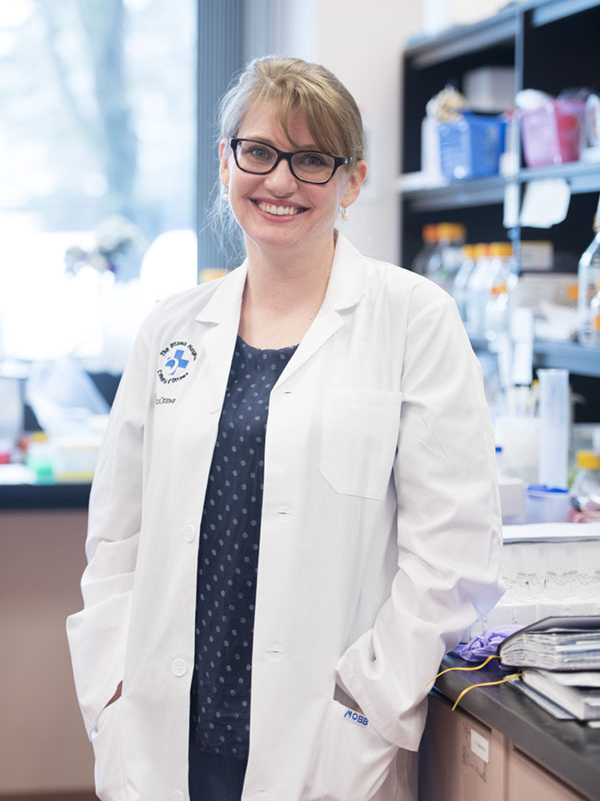
Dr. Julianna Tomlinson, the scientific program manager for the international team and co-director of research in the Schlossmacher Lab at our hospital, explains the importance of this study. “For us, this is an incredible opportunity to align efforts around the world, because it brings together scientists previously anchored in the PD field with researchers who heretofore have been working outside the field of Parkinson’s.”
There are eight institutes in five countries collaborating on this global study. It’s a unique opportunity to get answers to questions that scientists here in Ottawa have been asking for quite some time, including what role environmental triggers (other than toxins) play in Parkinson’s disease as they interact with genetics. “Right now, the treatments for Parkinson’s help the symptoms but they do not stop the progression of the disease. If we can identify disease processes at an early stage, then hopefully we will be able to stop or at least slow its progression before it reaches those later stages,” says Dr. Tomlinson.
The Ottawa Hospital leads this international effort
There are five main areas that this interdisciplinary and multinational study is pursuing. Our hospital’s focus is on how the immune system relates to Parkinson’s. Specifically, laboratory models will determine how viruses and bacteria could lead to changes in the body that are linked to pathology that is seen in the diseased human brain. Understanding the function of genes that are linked to Parkinson’s and whether those genes could be functioning in the immune system, rather than just in the brain, will also be explored.
The support of our hospital is instrumental in being able to lead this international effort. “There are so many people who are involved in making this work. It’s a full team effort, including financial officers, publication experts, and colleagues with knowledge in technology transfer,” explains Dr. Tomlinson.
Ultimately, it’s about finding answers for our patients and their family members who are desperately waiting for a breakthrough. As Dr. Schlossmacher explains, that’s why the world will be watching these scientists. “From an innovation and creativity perspective, we are setting the stage as a team as to how complex research avenues could be brought together, where people work collaboratively and constructively. We don’t undermine each other; we really complement each other and enable each other.”
Making the patient connection
For nearly two decades, Kelly McDonald felt there was something physically wrong with her, but even an eventual diagnosis of fibromyalgia in her 30s didn’t provide her with the answers she needed. McDonald, a professional photographer with a sharp eye, always knew something was off. Her stance wasn’t great, she struggled with her posture, and she’d get tired easily. However, solving her health mystery was an ongoing challenge and source of frustration. “You know, people think you’re a hypochondriac,” says Kelly.
It wouldn’t be until 2021, at the age of 52, when Kelly was diagnosed with Parkinson’s disease. In recent years, she started to develop tremors, her handwriting deteriorated, and she increasingly had a hard time getting her foot properly placed in her shoe. It was at that point, Kelly’s husband convinced her to see her doctor. Soon her right side became stiff and at times, she also felt numb. Kelly thought she was having a stroke.
“I consider myself a Parkinson’s warrior. I want to be a warrior. I want to bring more awareness to this disease, and I want people to be diagnosed earlier.”
– Kelly McDonald


give up.
When Kelly met with a neurologist at The Ottawa Hospital, tests revealed she had Parkinson’s — a diagnosis that she, surprisingly, welcomed. “I was just relieved, because I thought I was going to die from a stroke, like my dad did,” remembers Kelly.
Kelly’s father also had suffered from Parkinson’s. Moreover, soon after her diagnosis, she learned even more about her family history, namely that it also had affected the paternal side of her family. She is being cared for by Dr. David Grimes, the Head of the Division of Neurology at our hospital and an expert in movement disorders. It was Dr. Grimes who asked Kelly whether she would be interested in a study known as the Parkinson’s Progression Markers Initiative (PPMI).
Kelly admits that there were some dark days after her initial diagnosis. But in coming to terms with her new reality, she woke up one morning with a new view on her life. “I decided I have this, let’s do something good. I consider myself a Parkinson’s warrior. I want to be a warrior. I want to bring more awareness to this disease, and I want people to be diagnosed earlier,” explains Kelly.
“A lot of people start to tremor when they’re older, and some people think it’s a disease that only affects older people. But Michael J. Fox was diagnosed when he was 29.”
– Kelly McDonald
She enrolled in the PPMI study to help all those living with a Parkinson’s gene mutation, like her, that don’t realize they have it. It’s not until the shaking begins that the red flag goes up. “A lot of people start to tremor when they’re older and some people think it’s a disease that only affects older people. But Michael J. Fox was diagnosed when he was 29.”
What is PPMI?
PPMI is a landmark study led by The Michael J. Fox Foundation investigating better treatment options and prevention of the disease.
The Ottawa Hospital is one of nearly 50 sites across 12 countries participating in the expansion of the PPMI study. The team at our hospital is recruiting people recently diagnosed with Parkinson’s, who are not yet taking medication to control symptoms, as well as people age 60 and older who do not have Parkinson’s but are living with certain risk factors. Those interested in enrolling at The Ottawa Hospital can find the detailed eligibility criteria and how to contact the study team here. The Ottawa Hospital was the first Canadian study site to recruit participants when the study started to include sites outside the US; the expansion phase of the study means there could be 4,000 participants across all sites by the end of 2023.

“We are proud to be partnering with The Michael J. Fox Foundation and other PPMI site participants, and we are very grateful to the study’s dedicated volunteers who are helping us to move toward a future of disease prevention and better options for those living with Parkinson’s.”
– Dr. Tiago Mestre
Dr. Tiago Mestre is the principal investigator at our hospital, and he explains initial discoveries from this global study have already had an impact. “Early findings have revolutionized the understanding of Parkinson’s biology and the design of clinical trials testing potential new treatments, but there is much more to uncover. We are proud to be partnering with The Michael J. Fox Foundation and other PPMI site participants, and we are very grateful to the study’s dedicated volunteers who are helping us to move toward a future of disease prevention and better options for those living with Parkinson’s.”
Kelly joined the study mid-2021 and she’ll be monitored for 13 years. She says it’s been an amazing experience so far and she’d encourage others to consider joining. “Not only do you gain information about yourself and current information on your condition, but a study like this can help other people in the future. It also seems like Parkinson’s runs in my family. I could learn important information that could help my sister or my niece.” says Kelly.
For now, she’s looking ahead and doesn’t lose focus, whether it’s on her photography or as a warrior combatting Parkinson’s.
The Ottawa Hospital is a leading academic health, research, and learning hospital proudly affiliated with the University of Ottawa.