Published: December 2022
Content warning: Graphic description, in his own words, of the injuries he sustained.
Travis Vaughan shares the story of the night of December 18, 2019, when he arrived by air ambulance to The Ottawa Hospital Trauma Centre after a snowmobile crash in rural Ottawa that left him with life-threatening injuries. This is Travis’ story, told in his own words, about how our orthopaedic trauma team was ready to save his life.
It was a late afternoon on a Wednesday in December, and we just received our first real snowfall of the season. I was excited to get home from work to take the snowmobile out. My wife would be home from work soon, so I wasn’t planning on staying out long — just a quick loop and back home for the night. There was still light in the sky, but we were inching closer to the shortest day of the year.
I was on my way back — about 300 yards from the house — when the snowmobile hit a patch of very rough ground under the snow. As soon as the skis hit the frozen furrows of ground, the front end of the snowmobile broke apart. The machine rolled, taking me with it.
It all happened in the blink of an eye. While in the air, I remember being confused as to why the snowmobile suddenly upset, then I hit the ground hard.
“I’m grateful that through all of this, I was able to stay calm and keep my breathing steady, thanks to the reassuring support coming from the other end of the phone.”
– Travis Vaughan
Initially I didn’t think I was any worse for wear, until I looked down. My leg was torn wide open, and my femur was completely exposed — there was a lot of blood, but no pain. My adrenaline kicked in immediately. Luckily, I had stuffed my cellphone in my pocket and was able to dial 911. I explained to the calm voice of the operator that I was lying alone in a field just north of Almonte. She asked several questions, and I conveyed the severity of the situation, explaining my left leg was dangling and nearly detached. I was trying to make a tourniquet, but didn’t have a belt and wasn’t able to get my waist band torn out of my snow pants. I was acutely aware the situation was dire — if help didn’t arrive quickly, things would likely not end well. I remember her telling me there was all kinds of help on the way, and the Ornge air ambulance had been dispatched.
My hands started to numb from the bitter cold, and I wanted to call my wife, but the operator insisted I stay on the line until help arrived. I’m grateful that through all of this, I was able to stay calm and keep my breathing steady, thanks to the reassuring support coming from the other end of the phone.
Desperate for help to arrive
Unfortunately, the cold air caused my phone to die, cutting me off from the 911 operator. Sitting alone I remember thinking — you’re 32-years-old, this isn’t how it’s supposed to end. It was a surreal feeling. Strangely, it wasn’t scary — a warm calm sort of settled over my body. I remember thinking either I was going to hear sirens and see help coming, or I wasn’t, and this would be it. I started to think about my wife and family, and all the happy milestones I would miss.
But my next thought was different — and it hit me like a train — if I didn’t survive this, it would be my wife and family left to pick up the pieces, not me. I was furious with myself for succumbing to self pity while not thinking of how devastating and difficult this would be for my loved ones. This was the most intense thought I’ve ever experienced. From that moment on, I was going to give everything I had left to live; putting one hand in front of the other, I began to crawl. The next thing I knew, our dog came running towards me across the field. He looked at me with a what-did-you-do expression. He knew I was in trouble and stayed by my side as I slowly dragged myself home.
My wife, Jenn, and my brother, Tyler, who was living with us at the time, were both at home by the time I got to the house. I pushed open the door, and my wife turned and looked at me. I can still see the shock on her face. She came running towards me, grabbed me a belt and covered me with a blanket, before going to find my brother for help.
“From that moment on, I was going to give everything I had left to live, putting one hand in front of the other, I began to crawl.”
– Travis Vaughan

Tyler raced to make a tourniquet to help ease the blood loss; not many people could have done that, and I’m here because of it. Soon, the emergency responders started to arrive and they applied a proper tourniquet, started fluids, and worked to stabilize me. I was loaded into the ambulance — time was of the essence, so they quickly transported me to the awaiting air ambulance. The pilot had tried to land in the yard, however, due to trees and uneven ground, he had to set the helicopter down on the road. My memory starts to get a little fuzzy here, I’m so grateful to my wife, brother, the police officers, paramedics, and firefighters for the role they played in saving my life.
“When I say a team, it’s no exaggeration — my family told me there were close to 20 professionals ready and waiting. It was powerful to witness, and it’s not lost on me that because I was at a Level 1 Trauma Centre, I had immediate access to any equipment necessary. This level of care is unbelievable.”
– Travis Vaughan
Unbelievable care awaited me at the Trauma Centre
When we landed at The Ottawa Hospital’s Civic Campus a full team awaited me. When I say a team, it’s no exaggeration — my family told me there were close to 20 professionals ready and waiting. It was powerful to witness, and it’s not lost on me that because I was at a Level 1 Trauma Centre, I had immediate access to any equipment necessary. This level of care is unbelievable.

The team had received details of my injury while I was in the air. I remember feeling the first sigh of relief when we arrived — I was in good hands. My family was also in good hands, and that was equally comforting to hear afterwards. My wife received a phone call from a physician on the way to the hospital explaining what had already been done and what was planned. When my mother, sister, and wife arrived at the hospital, they were met by a social worker who was exceptional and again briefed them on all that was going on.
“It was my wife and brother that gave me my first fighting chance to live. Now, it was up to the trauma team to do the rest.”
– Travis Vaughan
It still amazes me to this day that I remember so much about that experience. I recall the faces of the trauma team as they did a full evaluation to determine if there were any other injuries. Each person acted quickly and concisely to get answers. I remember a CT scan showed I didn’t have any head trauma and my neck was fine — but I was hypothermic because of the extent of time I was outside.
The damage to my femur and surrounding tissue was extensive and critical. I recall someone saying the tourniquet Tyler put on my leg is likely the reason I made it to the hospital alive — it was my wife and brother that gave me my first fighting chance to live. Now, it was up to the trauma team to do the rest.

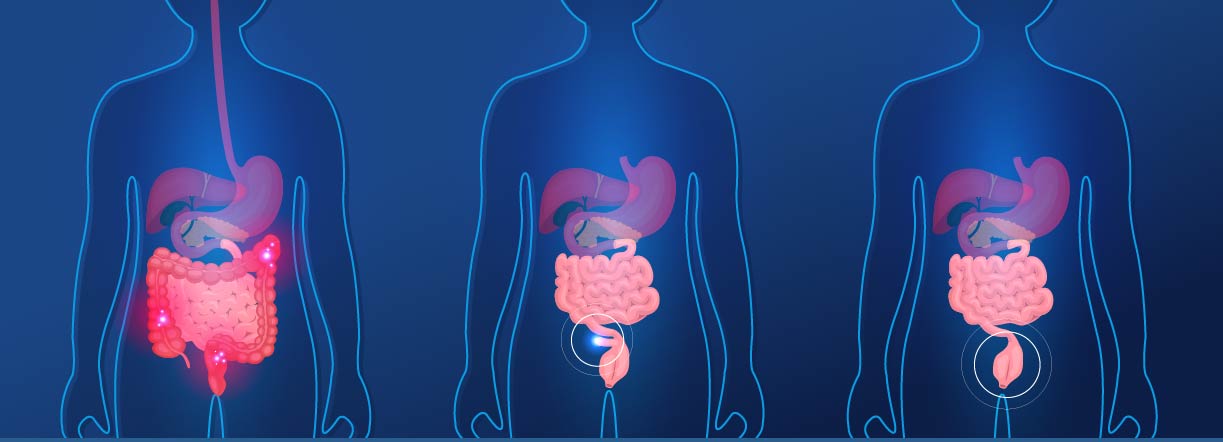
In 2021–2022, we admitted 992 patients for trauma care, up from 958 in 2020–2021.

40.3% of trauma patients in 2021–2022 were 65 or older.

Falls and motor vehicle collisions are the leading causes of injury at 43% and 33.8% respectively in 2021–2022.

67% of patients arrive directly from the scene, 33% from another facility.

Fracture cases annually: 3000+ (2000+ of these cases require hospitalization)
Orthopaedic trauma team gave me a chance at a full recovery
Getting the femur positioned back in my leg was going to be the first, and very painful, thing to do. Dr. Allan Liew, Director of Orthopaedic Trauma, was the lead, and I remember an orthopaedic resident was with me — standing right by my head. They explained how they had to try and put my femur back in my leg. The resident had a good sense of humour, which really helped in that moment, and he said to me, “Ok, this is going to suck.”
And it really did, but it had to be done to help put me on the right path to recovery. Later that night, once I was stabilized, Dr. Liew took me into surgery. I had a debridement — which is basically a thorough cleaning of the wound — and that’s when they realized there was some bone loss from the accident. What I mean by that is a piece of my femur was missing — still back in the field. So, my leg had to be stabilized with pins and bars just above the knee.
This whole surgery was crucial to reduce the risk of infection, and Dr. Liew did an incredible job with what he had to work with. That first surgery was critical in setting me up for a successful recovery.
I returned to the operating room on December 21 for another debridement, which gave my surgeons the chance to reassess how the tissues were doing, as well as the bone. Then four days later, on Christmas Eve, I had a third surgery — a definitive fix, as it was called. A plate and screws were used to stabilize my femur, but also, the surgical team needed to start the process to build back the missing bone. A block of bone cement was placed in the area where the bone was missing. Amazingly, the body will start to form a healing membrane around the cement, and six to eight weeks later I would return to have the block removed and a bone graft placed inside the membrane.

Orthopaedic trauma team gave me a chance at a full recovery
Getting the femur positioned back in my leg was going to be the first, and very painful, thing to do. Dr. Allan Liew, Director of Orthopaedic Trauma, was the lead, and I remember an orthopaedic resident was with me — standing right by my head. They explained how they had to try and put my femur back in my leg. The resident had a good sense of humour, which really helped in that moment, and he said to me, “Ok, this is going to suck.”

And it really did, but it had to be done to help put me on the right path to recovery. Later that night, once I was stabilized, Dr. Liew took me into surgery. I had a debridement — which is basically a thorough cleaning of the wound — and that’s when they realized there was some bone loss from the accident. What I mean by that is a piece of my femur was missing — still back in the field. So, my leg had to be stabilized with pins and bars just above the knee.
This whole surgery was crucial to reduce the risk of infection, and Dr. Liew did an incredible job with what he had to work with. That first surgery was critical in setting me up for a successful recovery.
I returned to the operating room on December 21 for another debridement, which gave my surgeons the chance to reassess how the tissues were doing, as well as the bone. Then four days later, on Christmas Eve, I had a third surgery — a definitive fix, as it was called. A plate and screws were used to stabilize my femur, but also, the surgical team needed to start the process to build back the missing bone. A block of bone cement was placed in the area where the bone was missing. Amazingly, the body will start to form a healing membrane around the cement, and six to eight weeks later I would return to have the block removed and a bone graft placed inside the membrane.
Finally, after 10 days in hospital, I was able to go home. While I missed Christmas with my family, they were always present at the hospital. Staff also went the extra mile to celebrate Christmas with me. I was lucky to be alive and hopeful The Ottawa Hospital’s specialist were setting me up for a full recovery. But my journey wasn’t over — one more big surgery awaited me.
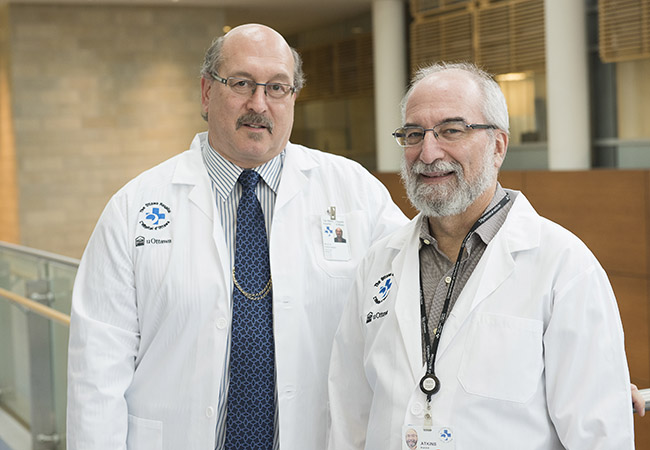
‘Superman’ surgeon leaves a lasting impression
That’s when I would meet Dr. Geoff Wilkin — or as I refer to him, Superman. He’s an orthopaedic surgeon who would lead that final surgery. Initially, the plan was for a short, routine surgery for bone grafting. However, after reviewing the imaging he wasn’t pleased with how my leg was healing and decided he wanted to re-align the femur — a redo if you will. Admittedly, I was shocked by this news. I had mentally prepared for a brief procedure, and now I was in for a six-hour surgery. But the truth was, I was having difficulty bending my knee, and Dr. Wilkin explained this was the best opportunity to get it right. If this wasn’t fixed properly, I would face a lifetime of issues that would impact my quality of life.
“Dr. Wilkin’s thoroughness and determination gave me the best chance at a future with a fully functional leg. He went so far past the extra mile to give me the best opportunity at recovery. He's given me a second lease on life — I will be forever grateful for that.”
– Travis Vaughan
On February 13, 2020 — just before COVID-19 hit our city — I was back in the operating room. Mine was a complex case. First, Dr. Wilkin had to remove that cement spacer in my femur. Then, he realigned the femur into a better position and attached two new plates to it. Up next was the bone grafting, where bone was harvested from my pelvis and placed in my thigh.
Dr. Wilkin’s thoroughness and determination gave me the best chance at a future with a fully functional leg. He went so far past the extra mile to give me the best opportunity at recovery. He’s given me a second lease on life — I will be forever grateful for that.


On to the best part. Thanks to the team that was waiting for me the night of the accident and those I would meet in the days and weeks ahead, including a long list of amazing nurses, I’m doing well. I don’t know that I’ll be skiing in the Rockies or running a marathon, but I was around to experience something far better. In October 2021, my wife and I welcomed our first child, a daughter. I now can chase her around the playground and enjoy any other activities she chooses to pursue growing up.
I’m beyond lucky to live in a city with access to the world-class care I received that cold December night. While my life hung in the balance, the trauma team was ready for me, and that’s something I will never forget.
Dr. Geoff Wilkin
Travis was one of those guys that every time I saw him, he was doing better and better. Despite everything he went through, his positive attitude and determination to get better never failed. Today, he's doing really well — he is enjoying an active life with his young family and his injury is largely a thing of the past. It feels great to have helped him get there.”