Update: Sadly, Ida Chen passed away on November 6, 2019. The following story was written earlier this year, after Ida had undergone fluorescence-guided surgery at The Ottawa Hospital.
Symptoms strike and reveal shocking brain cancer diagnosis
While out on a bike ride enjoying the warmth of Palm Beach, Florida, in December 2016, Ida Chen noticed something was wrong with one of her legs. She had experienced some minor symptoms in the weeks prior, but suddenly, her right leg stopped working. Unable to balance, she fell and couldn’t continue her ride.
The fall left her stunned. “After I fell, I could walk. It wasn’t a permanent issue,” said Ida. However, a gash in her leg sent her to a walk-in clinic near where she and her husband, Clarence Byrd, have their vacation property.
When Ida recounted what happened to the doctor, he assured her there wasn’t an infection in the leg but he was deeply concerned about what had led to the fall. He advised her to contact a neurologist.
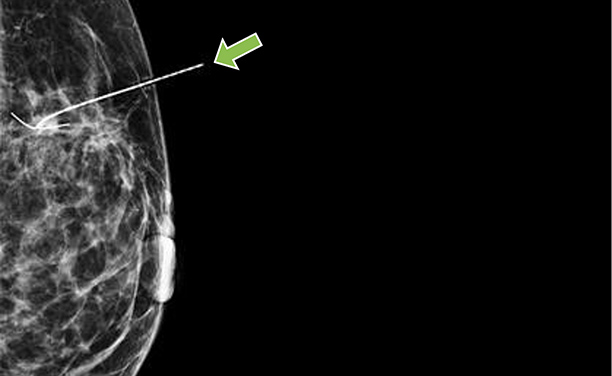
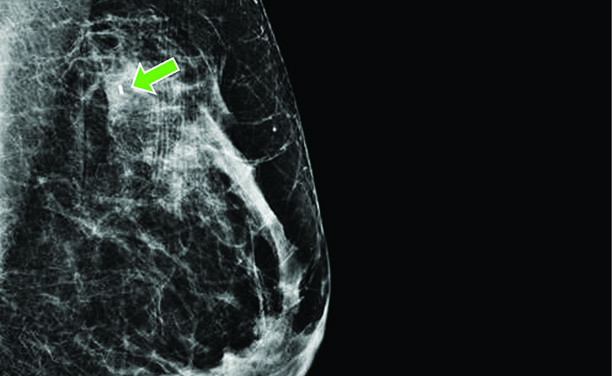
The neurologist scheduled an MRI, which revealed Ida had a 4 cm sized tumour in her brain which had features concerning for a malignancy. Recognizing that she may not survive a trip back to Canada for surgery, the neurologist contacted a neurosurgeon at the University of Miami Hospital who performed surgery only days later. Ida’s tumour was identified as a glioblastoma multiforme, an aggressive form of brain cancer. Unfortunately, not all the tumor could be completely removed, with 25% left behind due to the involvement of the tumor with the motor control areas for Ida’s leg.
Glioblastoma multiforme – brain cancer
For Clarence, it was hard news to absorb.
“It’s a particularly nasty cancer because it has fuzzy edges and they have trouble ensuring they get all of it.” Clarence Byrd, Ida’s husband
Ida advised her Ottawa doctor of the situation. Despite the fact that it was Christmastime, Dr. Lisa Lezack of the University of Ottawa Health Services made great efforts to ensure that when Ida returned to Canada, she would get prompt treatment.
Once back in Canada in early January, Ida was scheduled for radiation and chemotherapy. However, a new MRI showed that the tumour had returned to almost 100 percent of its original size.
Once again, just weeks after her first surgery, Ida was wheeled into the operating room, this time at The Ottawa Hospital under the care of neurosurgeon Dr. John Sinclair. It was a seven-hour surgery, followed by six weeks of radiation treatment and chemotherapy.
Ida’s initial prognosis was 12 – 15 months to live. Eighteen months after her diagnosis she had surpassed the odds, but the cancer was back, and she needed another surgery – her third in less than two years. This time, Dr. Sinclair had access to a revolutionary microscope, which was on loan to The Ottawa Hospital.

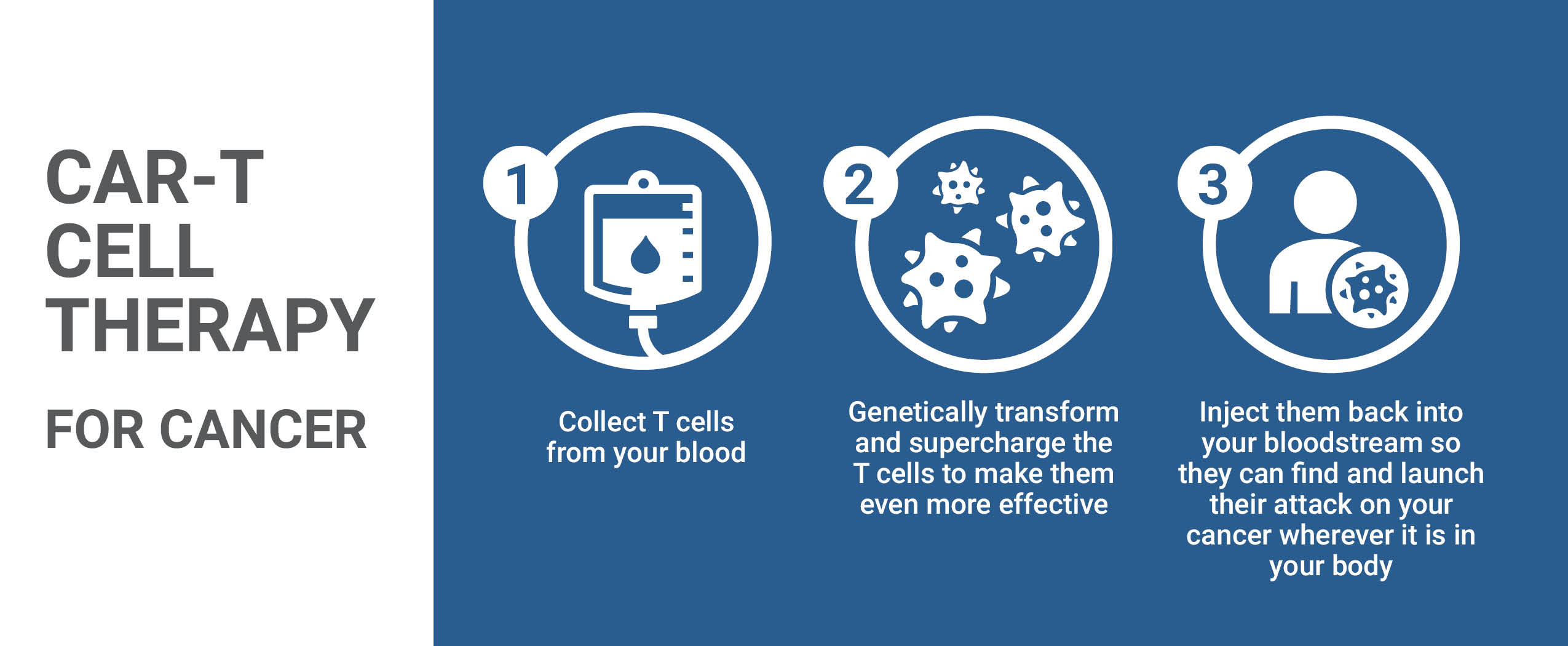
Illuminating cancer
Dr. Sinclair had traveled to Switzerland to receive training for fluorescence-guided brain surgery and was able to perform such surgery in the context of a trial using a microscope on loan to The Ottawa Hospital. The technique requires patients to drink a liquid containing 5-aminolevulinic acid (5-ALA) several hours before surgery. 5-ALA concentrates in the cancerous tissue and not in normal brain tissue. As a result, malignant gliomas “glow” a fluorescent pink color under a special blue wavelength of light generated by the microscope while the normal brain tissue does not fluoresce. This permits surgeons to achieve a complete resection of a tumour in many more patients, with recent studies demonstrating that this can now be achieved in 70% of surgeries as opposed to the previous 30% average.
“Seeing the brilliantly coloured tumours helps neurosurgeons remove more of the cancerous cells,” said Dr. Sinclair. “It’s like turning on the lights. You can actually see the difference between the tumour and the brain tissue. It’s dramatic.”
Added Dr. Sinclair, “Survival and quality of life are both dramatically impacted by this technology.”
In later discussions with Dr. Sinclair, it was clear that, without the use of the microscope Ida would have lost the use of her right leg. Ida explained, “He would have had to take out more of my brain matter and disable me to be sure he had all of the cancer cells.” She also learned that, because the microscope was available for a limited time on loan from the manufacturer, she was one of only ten people in Canada who benefited from the loan of the microscope.
Shortly after Ida’s surgery, a fundraising campaign was initiated to acquire a permanent microscope for Fluorescence Guided Surgery at The Ottawa Hospital. Recognizing how vital this piece of equipment was, Ida and Clarence made a substantial contribution towards its purchase. Dr. Sinclair performed the first surgery with the new microscope on August 26th.
“He saved my life.”
Thanks to the revolutionary care she received right here at home, Ida is enjoying a normal life style. “The Ottawa Hospital has given her outstanding service. Dr. Sinclair in particular has been very impressive,” said Clarence.
Ida is quick to add, “He saved my life. Twice.”
The Ottawa Hospital is a leading academic health, research, and learning hospital proudly affiliated with the University of Ottawa.