Published: September 2024
As the 100th anniversary of the Civic Campus inches closer — marking a century of care and medical breakthroughs — plans continue for the next 100 years of healthcare in our region. The final designs of the new hospital campus will come together in the next year. During this design phase, patients, leaders and staff at The Ottawa Hospital, Indigenous partners, and members of the community are all helping to refine the details of this new state-of-the-art health and research facility.
And while designs are finalized for the new hospital, construction of the parking garage to support the new campus is well underway.
Building a new hospital is a once-in-a-lifetime opportunity and it’s an opportunity that has business leaders, families, foundations, and many other community members stepping forward to support the $500-million Campaign to Create Tomorrow, which has raised an incredible $336-million to date in the region’s largest fundraising initiative.

Designing state-of-the-art operating rooms
The new campus will increase The Ottawa Hospital’s number of operating rooms (ORs) to help meet projected volume increases for surgeries in the future. These state-of-the-art ORs will be where some of the most life-changing care is delivered.
“It will enhance the patient experience and work efficiencies."
– Lisa Young
According to Lisa Young, Senior Planning Project Manager at The Ottawa Hospital, the functionality of that space will be key to accommodating not only more procedures, but also new equipment and technology. “It will enhance the patient experience and work efficiencies. We’re also focusing on the function of what the teams providing care do within these spaces, rather than the physical form of the building.”
Optimizing workflow in and around the ORs
Enhancements will include a bay of ‘block rooms’ where pre-surgery preparation can take place outside the main OR itself. These rooms can be used for patients receiving regional anesthesia before entering for surgery, helping reduce potential delays, and making the best use of time in the OR for both patients and care teams.
Dr. Sundaresan, Head of the Department of Surgery, and a clinical thoracic surgeon, explains that location of the ORs is vital for optimizing workflow, especially during critical moments. “The ORs at the new campus will be located next to the interventional radiology suites, which is exciting,” he says.

“When the new campus opens, we’ll have one of the most state-of-the-art surgical facilities in Canada, if not North America.”
– Dr. Sudhir Sundaresan
Interventional radiology is a medical specialty that performs minimally invasive treatments using x-ray imaging to guide small instruments, like catheters, through blood vessels and organs to treat a variety of diseases. “In the event there’s a complication during that procedure, sometimes the patient must go urgently into an OR. Now, the patient won’t have to be moved to another location to access the OR — it will be right there.”
New and emerging technologies will also enhance patient care. “When the new campus opens, we’ll have one of the most state-of-the-art surgical facilities in Canada, if not North America,” says Dr. Sundaresan. “Taking advantage of technology that will help us take surgery to the next level is one of the most exciting areas for development in the future.”
New neurosurgery rooms will come with innovative technology
Teams are also exploring innovative technologies such as an intraoperative MRI machine that captures real-time images of the brain during surgery.
Built on a rail system in the ceiling and considered a gold standard for procedures like brain tumor surgery, this MRI machine would be housed within the operating theatre, but just outside the operating room itself. If a patient needs imaging during a procedure, a door is opened, and the MRI can slide in on rails without having to relocate the patient with minimal disruption.
One of the goals in current design plans is for all ORs to have full audio video (AV) integration to help accommodate minimally invasive surgeries and for teaching purposes.
“Having AV integration in each suite provides more flexibility for patients,” Lisa explains. “We currently have specific rooms at each campus that can accommodate this, but having monitors and the ability to connect cameras in all of the ORs will be a new baseline of care that we could provide at the new campus.”
Digital solutions for a proactive approach to care

There are plenty of opportunities for technology to make a positive impact on patient care and experience.
“We’re striving to build on the digital experiences that people have in other areas of their lives to enhance the healthcare services we provide.”
– Glen Kearns
“We’re striving to build on the digital experiences that people have in other areas of their lives to enhance the healthcare services we provide,” says Glen Kearns, Executive Vice President and Chief Information Officer at The Ottawa Hospital. “Whether it’s inpatient care, preparing a patient before they even visit the hospital or following up with them at home, technology can offer solutions and more seamless care.”
Our hospital is also exploring the possibility of remote or virtual admissions to better support seamless inpatient and at-home care. The goal is to launch at the current campuses in advance, so it’s operationally ready on day one at the new campus.
“We want to leverage technology to reduce in-hospital admissions, wait times, and improve how patients interact with our teams.”
– Mathieu LeBreton
“We want to leverage technology to reduce in-hospital admissions, wait times, and improve how patients interact with our teams,” says Mathieu LeBreton, Senior Project Manager and Digital Experience Lead. “Ideally, we’ll have technology that enables and enhances workflow and reduces workflow burden on staff to improve their day-to-day experience.”
Mathieu adds that technology will be integrated to improve the experience of patients who are admitted. All rooms will be single patient and will have digital access so patients can stay connected with care providers and loved ones and access their health information, appointments, and entertainment. Throughout the new campus, technology can also help patients and visitors navigate the hospital.

The role of AI
In recent years, artificial intelligence (AI) has made great strides in becoming a useful and adaptable tool in the workplace. Our Digital Solutions team is already looking at innovative ways to harness the power of AI.
The Ottawa Hospital recently announced a trial of Dragon Ambient eXperience (DAX) Copilot which uses ambient, conversational, and generative AI to create draft clinical notes during patient appointments. With patient consent, it securely records and creates medical notes for the physician to review and approve. The Ottawa Hospital is the first in Canada to trial this innovative solution aimed at reducing physician burnout and time spent on administrative tasks and allowing physicians to spend more time interacting with patients providing care.
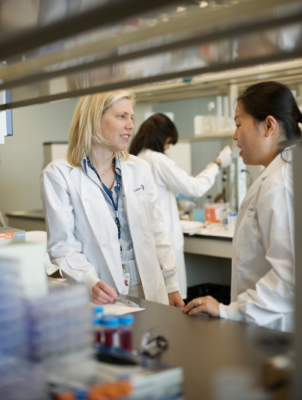
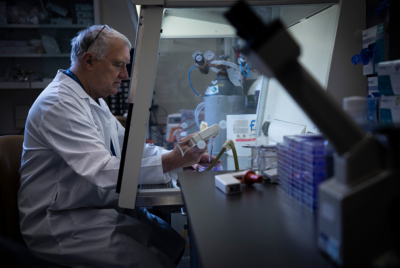
A hub for biotherapeutics research
The Ottawa Hospital is already a global research powerhouse, and the new campus will help take our research to unprecedented heights.
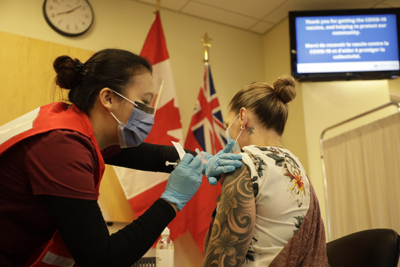
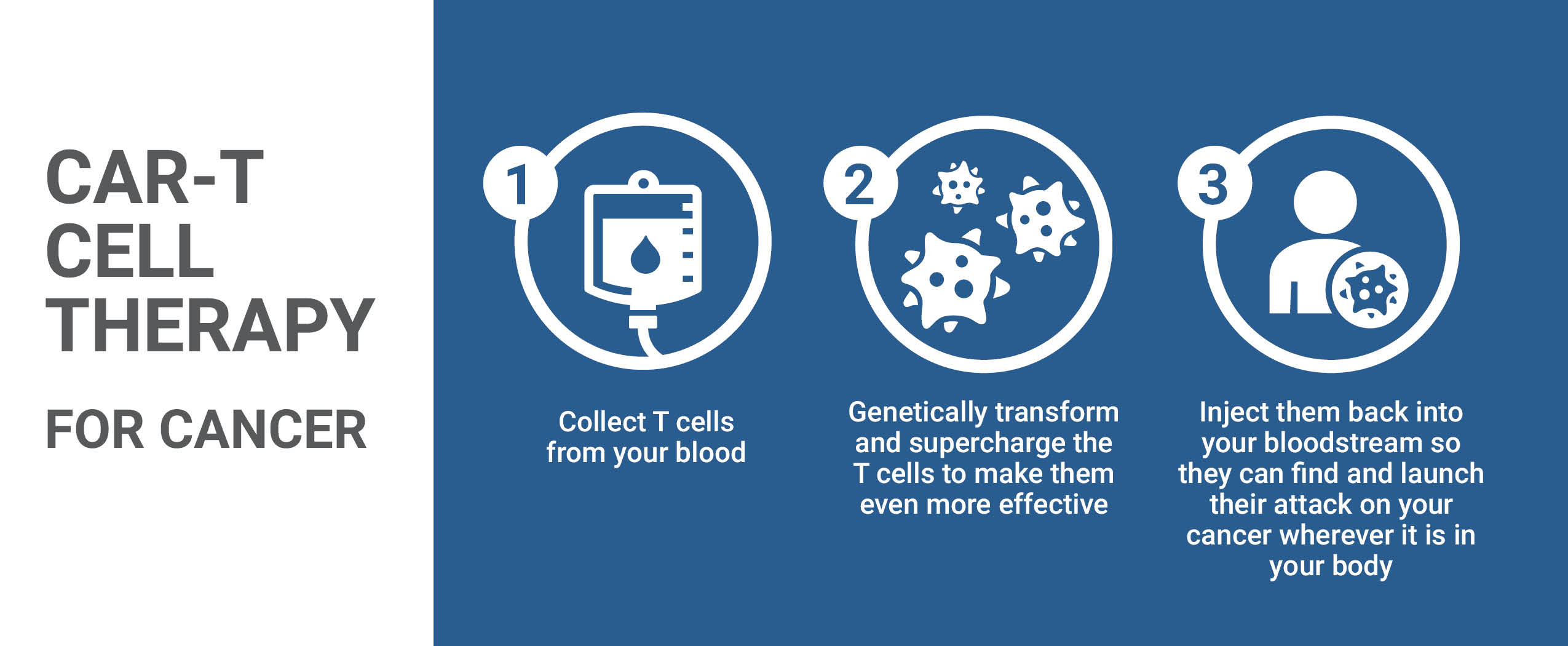
The expansion of the Biotherapeutics Manufacturing Centre (BMC) at the new campus will boost our capacity to develop and manufacture lifesaving biotherapeutics, including vaccines, gene therapies, and cell therapies right here in Ottawa.
Over the last 15 years, researchers at our hospital have led more than 20 world-first clinical trials using biotherapeutics such as stem cells, cancer-fighting viruses, and cellular immunotherapy. These trials are possible because the BMC is a specialized clean-room facility that develops and manufactures novel therapeutic products incorporating cells, genes, viruses, and other biological materials.
The BMC is the most experienced and successful facility of its kind in Canada, with more than 40 full-time staff currently based at the General Campus. It consistently operates at full capacity and is booked far in advance with both academic and industry clients — making this expansion vitally needed to further push the boundaries of research and bring more treatment options to patients.
Looking ahead to the next century of healthcare in Ottawa
When the Civic Campus first opened 100 years ago, the world had just emerged from a pandemic and the new hospital was considered the most modern in North America. Now, we find history repeating itself. We are witnessing the community rally together behind a historic campaign that will take research to the next level and help support the most modern and cutting-edge hospital campus in the country. This will transform the patient experience for generations to come, and we invite you to join us.