Originally published: January, 2022
When Owen Snider faced the news that his lymphoma had returned for the third time in ten years, he knew his options were running out. But a transformational new treatment known as CAR-T therapy gave him renewed hope. The Ottawa Hospital was recruiting patients for a clinical trial investigating a made-in-Canada approach to this cutting-edge treatment. He just needed to qualify for the trial.
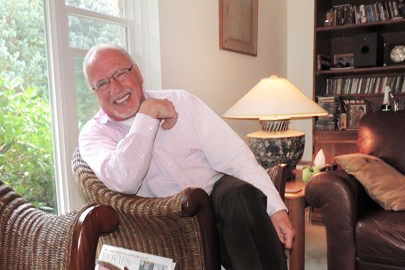
In 2010, Owen was diagnosed with large B-cell lymphoma. In his early 60s at the time, he went through a chemotherapy treatment known as R-CHOP. For most people, it lasts 18 weeks. “It was a rigorous treatment. I got through it okay and was six years clear, but then it came back — the lymphoma returned in 2016,” says Owen.
When the cancer returned, his care team at The Ottawa Hospital vetted him for a stem cell transplant. By the summer of that year, he went through what he called an intensive program using his own stem cells. A high dose of chemotherapy was used to remove harmful immune cells in preparation for the transplant of his own healthy cells. “It’s pretty brutal, and after two or three months of wishing maybe I wasn’t around, things improved. I was clear for another four years.”
“I was given five or six months to live. My wife and I were downhearted with that news.”
— Owen Snider
Lymphoma returns for a third time
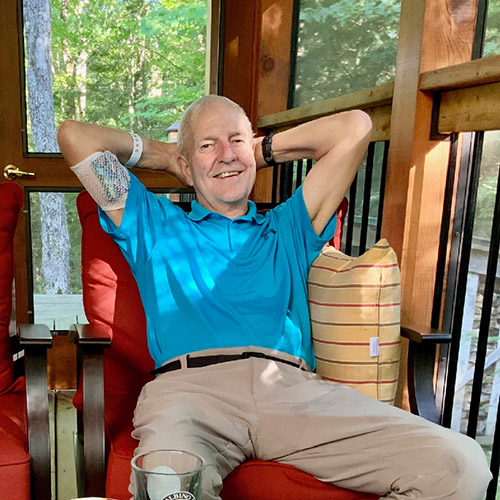
Following his stem cell transplant, Owen remained healthy for four years, enjoying retirement at his home in a beautiful, wooded area near Calabogie, where he lives with his wife, Judith Snider. But then Owen faced his biggest challenge yet when the lymphoma returned — again. This time, the diagnosis came in May 2020, in the midst of the pandemic. “I remember my oncologist saying they’ve done pretty much everything they could. I was given five or six months to live. My wife and I were downhearted with that news. I was basically going to be kept as comfortable as possible for six months,” remembers Owen.

However, one week later Owen received a lifeline. His oncologist called to say a CAR-T therapy clinical trial had opened at The Ottawa Hospital — a Canadian first. They wanted to see if he would be a good candidate. Throughout June of 2020, he went through a battery of tests and scans to see if he qualified for the trial.
“This type of immunotherapy research is groundbreaking, and it’s never been done in Canada before.”
– Dr. Natasha Kekre
By mid-June, Owen got the green light. He was a candidate for the clinical trial, and didn’t hesitate to enroll. “I either participate in the trial or I lie around here for four or five months waiting for the end. Which choice would you have made? The positive way to put it is that I was very excited to be a part of the trial. We’re the kind of people where the glass is always half-full,” explains Owen.
What is CAR-T therapy?
CAR T-cell therapy is a type of immune therapy that is an emerging biotherapeutic treatment that harnesses the power of a patient’s own immune cells, known as T-cells, to treat their cancer. T-cells play a critical role by killing abnormal cells, such as cells infected by germs or cancer cells. In some cancers, like lymphoma or leukemia, cancerous cells become invisible to the T-cells that are meant to kill them. In CAR-T therapy, the T-cells are collected and reprogrammed in the lab to recognize and destroy the cancerous cells.
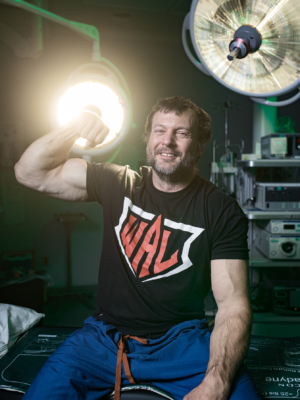
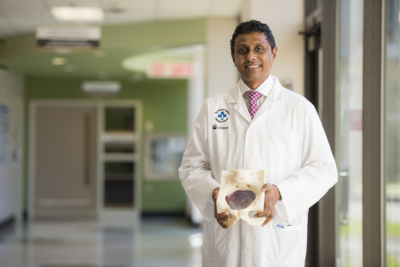
Dr. Natasha Kekre is a hematologist and associate scientist at The Ottawa Hospital. She is leading the development of Canada’s first CAR-T research platform in collaboration with the BC Cancer Centre. “This type of immunotherapy research is groundbreaking, and it’s never been done in Canada before. This is a therapy that uses a patient’s own immune system. It’s personalized medicine — it’s very individualized to each patient,” explains Dr. Kekre.
The Ottawa Hospital is one of the first hospitals in Canada to participate in nationally-led CAR-T trials, and as one of Canada’s top research and treatment centres, the hospital is ideally positioned to play a lead role in bringing an innovative CAR-T research program to Canada, and to Canadian patients.
Going for the Pac-Man effect
In late June 2020, Owen went through apheresis which is the process of withdrawing the T-cells in his blood. “They put an IV in my right arm, and ran the tubing through the machine, and the machine processes the blood and pumps it back through the tubing into my other arm. I lay there on the bed for three or four hours, without moving I should add.”
“It’s just like Pac-Man, the modified T-cells ran around in my blood stream, chomping away at the lymphoma.”
– Owen Snider
Those T-cells were then sent to a lab in BC, re-programmed, and then returned to our hospital two weeks later. Then the T-cells were re-administered just like a blood transfusion. “It allows for that new immune therapy in these cells to go and find the patient’s cancer cells, attack them, and kill them. And it also stimulates the immune system in that patient to further go attack and fight their cancer,” explains Dr. Kekre.
On July 2, Owen received a PICC line and then went through three days of chemotherapy. Four days later he was re-injected with his T-cells and they got to work. “It’s just like Pac-Man, the modified T-cells ran around in my bloodstream, chomping away at the lymphoma.”
His re-programmed T-cells were specifically looking for cancer cells to kill. Owen would need to wait to find out if it was working.
Did the CAR T-cells therapy work?
One month later, Owen and Judith received some exceptional news. “At my check-up 30 days after getting my T-cells back, I was almost clear of cancer. The scan showed that there was almost nothing left. I was gobsmacked,” he says.
By the three-month mark, Owen says he was as “clean as a whistle.” Eighteen months later, there is still no sign of lymphoma.
For Dr. Kekre, giving patients like Owen new hope for the future is what inspires her. “For the first time, I think in a long time, Owen felt that the lymphoma might actually be disappearing. He’s had multiple scans since then that show the same thing. And so now, I think he’s starting to believe it. And I think that’s the reality of why I do this, because patients like him who had no options before, could soon have the option of CAR-T therapy. That’s what happened for Owen and that’s what we hope will happen for many more patients,” says Dr. Kekre.

What’s next for the clinical trial?
Dr. Kekre and her team are monitoring all patients enrolled in the trial and published preliminary results in June 2022. The purpose of the clinical trial is to provide proof to Health Canada this therapy is safe. “The reality is that we have a data safety monitoring board, which watches for the safety of the trial, and they’ve had no concerns. So, from a safety point of view, we’re very happy with the trial. And that’s why we are still open and we’re still able to enroll more patients,” explains Dr. Kekre.
Why is The Ottawa Hospital unique in its CAR-T therapy?
CAR-T therapy needs to be individually manufactured for each patient using the patient’s own cells combined with large amounts of highly pure virus to deliver the chimeric antigen receptors (CAR) gene. The Ottawa Hospital’s Biotherapeutics Manufacturing Centre is ideally positioned to manufacture the clinical grade virus needed to create CAR T-cells for clinical trials. In fact, we have the only facility in Canada that has produced this kind of virus for clinical trials.
The hope is that one-day CAR T-cell therapy may also be a treatment for a variety of cancers. “The world is watching us,” explains Dr. Kekre. “We’ve had a lot of attention from Denmark, and a few other European countries are reaching out. They believe in a system similar to ours, where patients all have the right to access healthcare. If CAR T-cells are here to stay, they have to be done in a sustainable approach for our patients. And that’s a big part of what we are building — this is only the beginning. And that’s what people are looking at us to see how we do it.”
“Without philanthropy, we wouldn’t have a Biotherapeutics Manufacturing Centre or a Methods Centre at The Ottawa Hospital, and we wouldn’t be able to do innovative clinical trials like this.”
– Dr. Natasha Kekre
This made-in-Canada CAR T-cell research platform will give Canadian patients more access to innovative clinical trials. “Canadian cancer patients shouldn’t have to wait for the research to be done elsewhere but be able to participate in innovative clinical trials here at home,” says Dr. Kekre.
Grateful for each day and philanthropic support for research
Today, Owen appreciates each day and a good quality of life thanks to the clinical trial. He feels strong and can’t wait for the day when he and Judith can travel again — grateful for the lifesaving research. “It was an honour and a privilege to be chosen for the trial.”
He also credits the extraordinary care team and those special moments when he visited the hospital. “I can tell you that I always felt more than comfortable. I felt encouraged by anyone I met. The team on 5 West as we know it, is wonderful. I had an occasion to go back there last spring, and it was like walking back into Cheers — everybody knows your name.”
As a longtime supporter of The Ottawa Hospital, and to see philanthropy play an important role in making this clinical trial a reality, he’s an even bigger advocate for encouraging support for our hospital. “All I can say is that the core funding of hospitals doesn’t provide for some of the innovative and cutting-edge things that go on, or maybe some really specialized piece of equipment. And that’s where the community donor can help and contribute to that effort.”

For Dr. Kekre, philanthropy provides the spark for clinical trials like this, and can help to keep them moving forward. “Without philanthropy, we wouldn’t have a Biotherapeutics Manufacturing Centre or a Methods Centre at The Ottawa Hospital, and we wouldn’t be able to do innovative clinical trials like this. We need this kind of research to get to a place where all Canadians can benefit from these therapies. Without philanthropy, we would never get there.”
And to Dr. Kekre, her team, and their collective efforts to give more patients hope, Owen has a simple message: “Thank you. The whole program is outstanding.”
About the Canadian-Led Immunotherapies in Cancer (CLIC) research program
The CLIC research program, established in 2016, brings researchers, clinicians and patients from across Canada together to build Canadian expertise and capacity for innovation in the promising field of cellular immunotherapy for cancer, including CAR-T therapy. The first CLIC clinical trial launched in 2019 at The Ottawa Hospital and at BC Cancer, with support from BioCanRx, BC Cancer, The Ottawa Hospital Foundation and the Ontario Institute for Cancer Research. Core facilities and resources supporting CLIC include The Ottawa Hospital’s Biotherapeutics Manufacturing Centre, BC Cancer’s Conconi Family Immunotherapy Lab, the Ottawa Methods Centre and the Blueprint Translational Research Group. CLIC team investigators include Drs. Natasha Kekre, Harold Atkins, John Bell, Kevin Hay, Rob Holt, Brad Nelson, John Webb, Manoj Lalu, Kednapa Thavorn, Dean Fergusson, Justin Presseau and Jen Quizi.
The Ottawa Hospital is a leading academic health, research, and learning hospital proudly affiliated with the University of Ottawa.